International experts provide a guide for rapid decision-making focused on transcatheter options

The first comprehensive clinical guidance on the diagnosis and management of acute heart failure caused by valvular heart disease is available, recently published as a review article in the European Journal of Heart Failure
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“In the absence of guidelines, we sought to create a reference document for clinicians who must make rapid decisions when a patient with valve disease suddenly destabilizes,” says Samir Kapadia, MD, Chair of Cardiovascular Medicine at Cleveland Clinic and a member of the international writing committee that developed the document. “It will help less-experienced physicians formulate their thinking and decide on a treatment strategy, but even experts will find it interesting and valuable.”
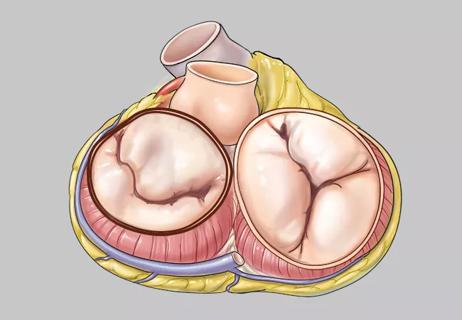
The writing committee — made up of interventional cardiologists, cardiac surgeons and cardiac imaging specialists — conducted a review of literature published between January 1994 and December 2023 that addressed acute heart failure caused by any of four valve diseases:
They aimed to reach consensus on current best practices for the management of each valve disorder, with an emphasis on transcatheter interventions.
“Clinical practice is accelerating beyond general appreciation and outstripping evidence from randomized controlled trials,” says Bernard Prendergast, DM, FRCP, another member of the writing committee and Chair of Cardiology at Cleveland Clinic London. “This has led to an imbalance in the understanding of how transcatheter solutions can help patients with decompensated heart failure. This review article reflects what’s going on in specialized centers like Cleveland Clinic.”
Valvular heart disease is typically a chronic problem characterized by gradual valve degeneration and progressively worsening symptoms. However, a small percentage of patients develop symptoms of acute heart failure resulting from rapid hemodynamic changes and subsequent decline in cardiac function.
Advertisement
“The chronic problem can become acute when an arrhythmia, an infection or a medical issue such as coronary artery disease or kidney failure pushes the patient over the edge,” Dr. Kapadia says. “With early intervention, some of these cases are reversible, but delay may cause the patient to rapidly spiral downwards.”
“Valve disease should not be underestimated,” Professor Prendergast adds. “One may think there is time to make the diagnosis, agree on a management plan and then intervene. In reality, stable disease can destabilize suddenly.”
To help physicians recognize the early signs of decompensation and understand how to confirm the diagnosis and proceed with appropriate treatment, the paper provides algorithms for all four disease entities it covers.
“When you make the decision to intervene, you should not delay,” Professor Prendergast says. “Providing access to a valve specialist and imaging specialist for assessment is essential.”
“Multidisciplinary teams are key to treating these patients,” Dr. Kapadia adds. “Treatment becomes a clinical decision because guidelines are not available.”
Previously, valve repair or replacement required open-heart surgery, even in patients with decompensated heart failure. Because decompensated patients are high-risk surgical candidates, attempts would be made to stabilize them with medications or device therapy (e.g., extracorporeal membrane oxygenation, intravascular microaxial blood pump, balloon pump) until they were strong enough to undergo surgery.
Advertisement
Today, mechanical bridges to surgery are rarely used in such patients because defective valves often can be corrected percutaneously.
“There are many interventional procedures — even definitive therapies — that can be performed at an acceptable risk,” Dr. Kapadia notes.
Success with transcatheter interventions is prompting physicians to reconsider strategies for treating certain patient populations with acute heart failure caused by valve disease. Younger patients with aortic stenosis are a good example.
“Traditionally, these patients would undergo open-heart surgery to replace their aortic valve,” Professor Prendergast says. “However, if they deteriorate dramatically, and their life can be saved by transcatheter aortic valve replacement (TAVR), there’s no harm in doing TAVR now and then doing a surgical valve replacement a few years later.”
Because most patients with acute decompensation are treated in the intensive care unit (ICU), the review’s algorithms specify which medications and mechanical treatments delivered in the ICU are most likely to be effective in stabilizing or reversing the disease.
Cleveland Clinic data have shown that patients with valvular cardiogenic shock, particularly from aortic stenosis, tend to be sicker than other patients in the ICU (JACC Adv. 2024;3[11]:101303). The complexity of treatment involved in caring for patients like these compelled Cleveland Clinic to start a critical care cardiology fellowship for cardiologists with a specialty interest in salvaging acutely ill patients. Three graduates of the fellowship have since joined the Cleveland Clinic staff.
Advertisement
The literature review revealed gaps in knowledge that must be addressed before formal guidelines on this topic can be developed, the review’s authors note. Cleveland Clinic is actively seeking to fill many of the gaps through database studies, as prospective studies are difficult due to the nature of acute decompensation. Nevertheless, the results should inform practice in disease-specific international guidelines that may be released within the next year, with U.S. guidelines to follow.
“We hope this article will stimulate more thinking and greater collaboration in quality observational studies and high-quality registries,” Professor Prendergast says.
“We should not give up on these acutely ill patients,” Dr. Kapadia notes. “There are many treatment options. Mortality may still be high, but there’s a very good chance we can help these patients.”
“With the advent of new technologies and expertise, we have a comprehensive approach to patients in heart failure caused by valvular disease,” adds A. Marc Gillinov, MD, Chair of Thoracic and Cardiovascular Surgery at Cleveland Clinic. “Working as a heart team, we now have many more options to enable successful treatments.”
Advertisement
Advertisement

Join us in Florida this winter for a long-standing CME favorite
Join us in New York Dec. 6-7 for broadened version of a CME crowd-pleaser

Infant with complex congenital heart anomalies thriving after biventricular circulation is restored
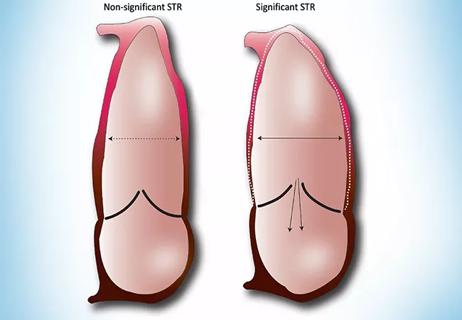
New study illuminates mechanical underpinnings of secondary leaks

Optimal management requires an experienced center

A closer look at the impact on procedures and patient outcomes

Multidisciplinary care can make arthroplasty a safe option even for patients with low ejection fraction

Experts are challenging the one-size-fits-all paradigm