New study illuminates mechanical underpinnings of secondary leaks
Pulmonary arterial hypertension (PAH) is known to be associated with secondary tricuspid regurgitation (STR). Simultaneous presence of the two conditions portends a poor outcome, but why some patients develop STR and others do not is unclear.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The answer may lie in new research by Cleveland Clinic cardiologists and pulmonologists, who compared functional, anatomic and hemodynamic characteristics between patients with PAH who did and did not develop STR. Results of the study (Am J Cardiol. 2022;175:97-105) suggest that the key is right ventricular (RV) shape and function, not the anatomy of the tricuspid valve.
“Those who had worse RV function and more spherical RV shape tended to develop more significant TR,” says cardiologist Serge Harb, MD, the study’s corresponding author. “Interestingly, the hemodynamic data — and specifically the right atrial pressure, rather than imaging data — were predictive of clinical outcomes.”
According to Dr. Harb and his co-authors, theirs is the first analysis to combine data from transthoracic echocardiography (TTE), cardiac computed tomography (CCT) and right heart catheterization (RHC) in an attempt to tease out the complex determinants of significant STR in patients with PAH. For the study, the two conditions were guideline-defined at the time patients were selected and the researchers also looked at long-term outcomes in the cohort.
Data from the Cleveland Clinic Pulmonary Hypertension Registry formed the basis of the retrospective study. Eligible patients were those diagnosed with PAH between 2007 and 2013 who had mean pulmonary artery pressure ≥ 25 mmHg, mean pulmonary arterial wedge pressure ≤ 15 mmHg and mean pulmonary vascular resistance ≥ 3 Wood units by RHC.
Eighty-eight patients were included in the cohort, 52 of whom had significant STR (28 moderate and 24 severe), as defined by absence of primary tricuspid valve leaflet pathology on TTE. Median age was 57 years, and 78% were women.
Advertisement
Median time between TTE and CCT was 1.1 months and between CCT and RHC was 1.45 months. The patients with and without STR did not differ in baseline characteristics, including atrial fibrillation.
The researchers found that the two groups had similar clinical characteristics and, to their surprise, tricuspid annular anatomic features. Although they hypothesized that anomalies in the tricuspid valve were responsible for regurgitation, that was not the case.
“We thought that changes in the tricuspid valve would explain the leak, but it turned out that because the right ventricle supports the tricuspid valve apparatus, its shape and how it deformed were key,” Dr. Harb explains. “The other interesting finding was that the hemodynamic data were more predictive of outcome than the imaging data.”
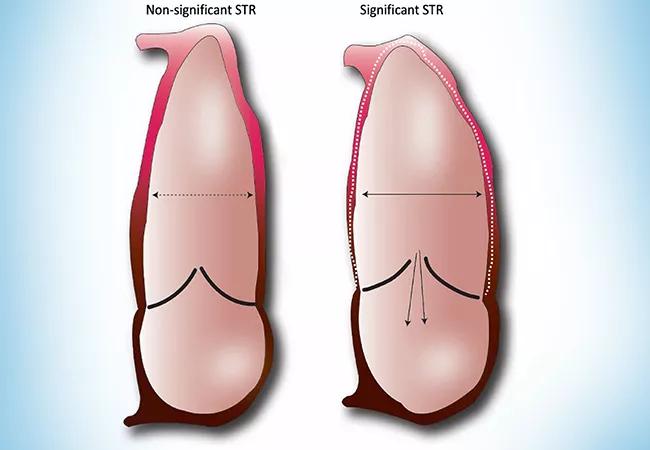
TTE analysis showed that patients with (versus without) significant STR had worse RV dysfunction (tricuspid annular planar systolic excursion = 1.5 vs. 2.1 cm; P = 0.02) as well as increased RV sphericity (sphericity index = 1.8 vs. 2; P = 0.004). In contrast, annular dimensions and shape were similar between the two groups, as were tenting heights and the lengths and angles of the mural and septal leaflets.
CCT analysis showed that tricuspid annular dimensions were similar between the groups, whereas patients with significant STR had higher right/left ventricular ratio (P=0.003). RHC showed that stroke volume and cardiac index were lower in patients with significant STR.
After controlling for age, gender and atrial fibrillation in multivariable logistic regression analysis, the authors found that the only imaging parameter independently correlated with the presence of significant STR was a fractional area change < 34% on TTE.
Advertisement
Multivariable analysis revealed that after a median of 54 months, right atrial mean pressure was the only factor independently associated with the composite outcome of all-cause mortality and hospitalization for PAH (Figure).
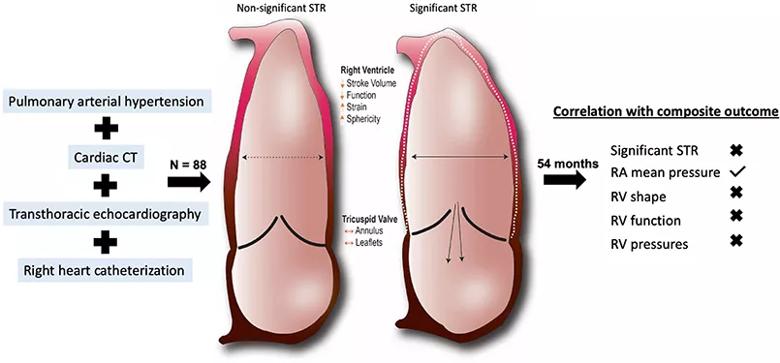
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ea0608a2-45dc-40d0-8faa-ae34996776d7/22-HVI-3135510-CQD-inset_jpg)
Figure. Insights into the mechanisms and clinical context of secondary tricuspid regurgitation (STR) in pulmonary arterial hypertension. Anatomic and functional alterations in the right ventricle (RV) are implicated in the development of significant STR in patients with pulmonary arterial hypertension, yet these measures had no impact on survival in this cohort. Using transthoracic echocardiography, cardiac CT and right-sided cardiac catheterization, the sole feature that predicted the composite outcome of all-cause mortality and hospitalization for pulmonary arterial hypertension was right atrial (RA) mean pressure (hazard ratio = 1.07 [1.01, 1.14]; P = 0.02). Reprinted from American Journal of Cardiology (2022;175:97-105) ©2022, with permission from Elsevier.
Taken together, according to Dr. Harb, the results show that multimodality imaging provides insight into the mechanistic changes that lead to STR development in patients with PAH — namely, RV rather than tricuspid annular changes — and that hemodynamic data provide important prognostic information.
“Clinicians should not think about tricuspid regurgitation as a function of only the valve itself,” he says. “Rather, the annulus and leaflets can function properly as an apparatus only in concert with the right-sided chambers of the heart. Combining multimodality imaging with hemodynamic parameters obtained by RHC, as we did in this study, may have potential for risk-stratifying patients with PAH.”
Advertisement
“We demonstrated that both worse RV function and more pronounced sphericity — as opposed to intrinsic valvular disease — are linked to the development of significant tricuspid regurgitation,” adds study co-author Adriano Tonelli, MD, of Cleveland Clinic’s Department of Pulmonary Medicine. “These novel findings are very important to help answer why the severity of tricuspid regurgitation decreases as RV function recovers, either with effective PAH-specific therapies or lung transplantation.”
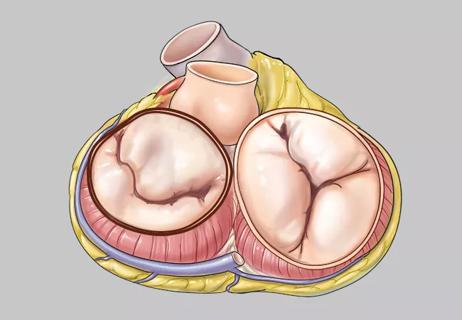
“This is a fascinating mechanistic study that tells us we need to pay more attention to the intrinsic RV function, remodeling and hemodynamics in the assessment of patients with PAH and secondary TR,” observes Patrick Collier, MD, PhD, a cardiologist in Cleveland Clinic’s Section of Cardiovascular Imaging who was not involved in the study. “Different from the left side, the valves of the right ventricle are not continuous. While secondary mitral regurgitation is highly dependent on systolic blood pressure, this study may help explain why not every patient with PAH develops secondary tricuspid regurgitation.”
Advertisement
Advertisement

Join us in Florida this winter for a long-standing CME favorite

International experts provide a guide for rapid decision-making focused on transcatheter options
Join us in New York Dec. 6-7 for broadened version of a CME crowd-pleaser

Infant with complex congenital heart anomalies thriving after biventricular circulation is restored

Optimal management requires an experienced center

A review of treatment options for patients who may not qualify for surgery

A closer look at the impact on procedures and patient outcomes

Collaborative patient care, advanced imaging techniques support safer immunotherapy management