Inflammation found more predictive of events than LDL-C in pooled analysis of RCTs
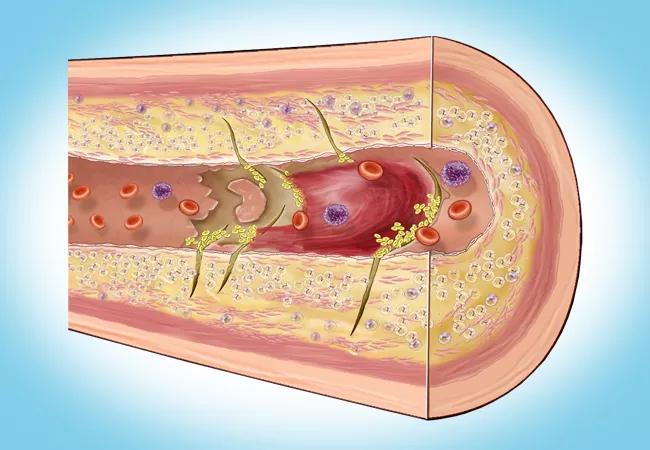
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c8ddc73a-9424-4eea-98cd-73748c54a111/23-HVI-3606661_atherosclerosis_650x450_jpg)
23-HVI-3606661_atherosclerosis_650x450
Vascular inflammation is a stronger predictor of residual cardiovascular risk than LDL cholesterol (LDL-C) level among statin-treated patients with atherosclerotic risk, according to a pooled analysis of three contemporary randomized controlled cardiovascular outcome trials comprising over 31,000 patients.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“These data tell us that if we want to further reduce risk of cardiovascular events in patients on statin therapy, we need to target inflammation,” says Steven Nissen, MD, senior author of the analysis, which was presented as a late-breaking clinical trial at the American College of Cardiology’s annual scientific session and simultaneously published online in The Lancet.
“Even after we’ve treated patients with very effective doses of statins, they still have some residual risk of a major cardiovascular event,” says Dr. Nissen, Chief Academic Officer of Cleveland Clinic’s Heart, Vascular & Thoracic Institute. “We conducted this study to determine what is the best way to target that residual risk — by further lowering LDL-C or by reducing inflammation as measured by high-sensitivity C-reactive protein (hsCRP).”
To address that question, Dr. Nissen was part of a multicenter team led by Paul Ridker, MD, that pooled data from three recent randomized controlled trials assessing adjunctive lipid-lowering therapy in patients on maximally tolerated statin therapy for primary or secondary cardiovascular prevention:
These cohorts were chosen, the investigators write, because “all three trials were conducted in the setting of intensive guideline-directed medical therapy and participants consequently had levels of hsCRP and LDL-C representative of contemporary statin-treated populations,” making them ideal for assessment of residual risk. “The patient populations of these studies were remarkably similar,” Dr. Nissen notes.
Advertisement
After pooling data from these studies’ collective 31,245 patients, the researchers assessed increasing quartiles of baseline hsCRP, a biomarker of residual inflammatory risk, and of LDL-C, a biomarker of residual cholesterol risk, in terms of their ability to predict future major adverse cardiovascular events (MACE), cardiovascular mortality and all-cause mortality.
Hazard ratios (HRs) for these end points were calculated across quartiles of hsCRP and LDL-C after adjustment for age, gender, body mass index, smoking, blood pressure, history of cardiovascular disease and randomization assignment.
The researchers found that residual inflammatory risk was significantly associated with all three primary end points, as follows:
In contrast, the relationship of residual cholesterol risk to the primary end points was neutral for MACE and of lower magnitude (relative to residual inflammatory risk) for both cardiovascular and all-cause mortality. Specific hazard ratios were as follows:
Advertisement
Notably, the observed ranges for hsCRP and LDL-C were virtually identical among the three trials, as were the relationships of each biomarker to future event rates.
In their study report, the investigators conclude that “targeting LDL-C alone is unlikely to completely reduce atherosclerotic risk and that inflammatory pathways have yet to be fully exploited” to reduce adverse cardiovascular outcomes. They add that combined use of potent lipid-lowering therapies and inflammation-inhibiting therapies — a strategy under investigation in several ongoing clinical trials — may become a future standard of care for atherosclerotic disease.
“This study is telling us we need to target inflammation for further risk reduction after LDL-C is well controlled,” Dr. Nissen observes. “There are some interesting therapies in development for that purpose, and we hope this study will accelerate those programs.” Such therapies include direct inhibitors of the NLRP3 inflammasome and interleukin-6 inhibitors. The study authors also note the potential of existing therapies such as SGLT2 inhibitors, GLP-1 receptor agonists and bempedoic acid, due to these agents’ hsCRP-lowering effects.
As noted in the published study, three randomized trials have already found that targeted anti-inflammatory therapy with canakinumab or colchicine significantly reduces cardiovascular events in statin recipients in the absence of further LDL-C reduction. Although one of these agents — oral colchicine — is available in inexpensive generic forms, its use for atherosclerosis has been modest. Dr. Nissen attributes this to the relatively small size of the studies supporting its effects on vascular inflammation and the absence of promotion of the drug due to its off-patent status.
Advertisement
His practice is to consider using colchicine in patients who have a low LDL-C but an hsCRP level greater than 2.0 mg/dL. “At Cleveland Clinic, we routinely measure high-sensitivity CRP when we order a lipid panel, and this helps determine potential need for anti-inflammatory therapy,” he says. “This study adds support to that practice.”
“Preventive cardiologists are always thinking about how to lower residual cardiovascular risk, particularly in our high-risk patients,” says Luke Laffin, MD, staff in Cleveland Clinic’s Section of Preventive Cardiology, who wasn’t involved in the study. “Statins provide the backbone of therapy in this group, and their risk reduction is derived not only from LDL-C lowering but also from anti-inflammatory effects.
“Physicians are increasingly aggressive at lowering LDL-C if it remains elevated even with statin therapy because of the wide availability of newer lipid-lowering therapies,” Dr. Laffin continues. “Cardiologists in general need to become better at assessing and considering residual inflammatory risk, in addition to residual LDL-C-associated risk, to best care for our patients. Medications that lower inflammation such as colchicine are available, but they have not yet been fully embraced. Moreover, the anti-inflammatory effects of SGLT2 inhibitors and GLP-1 receptor agonists may explain some these agents’ cardiovascular benefits.”
Advertisement
Advertisement
Cleveland Clinic pioneers a new paradigm in cardiovascular care delivery
Site visits offer firsthand lessons in clinical and operational excellence in cardiovascular care
Cancer drug helps treat decades-long symptoms in patient with complicated lymphatic issue
Findings support emphasis on markers of frailty related to, but not dependent on, age
Findings establish overweight/obesity as a modifiable risk factor for cardiovascular disease
Observational study supports adding CAC score to traditional risk factors for precision medicine approach
Visual snapshots of how we manage challenging cases
How our HVTI Advisory Services team facilitated swift improvements for an affiliated health organization