Surgeons recount the instant the OR went from hush to collective sigh

For the surgeons who performed Cleveland Clinic’s third face transplant — and first total face transplant — one moment from the 31-hour operation stands out from the rest.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“The crux of the surgery was after we had delivered the donor face to the recipient all in one unit and had completed the laborious work of attaching the many, many small blood vessels between the donor and recipient,” says Francis (Frank) Papay, MD, who led the transplant surgery team in the OR along with Brian Gastman, MD. The complexity and extent of vessel dissection, which notably included the internal maxillary artery, was one of the transplant’s points of distinction, as detailed in this overview of the procedure and the recipient’s remarkable case.
“You then reach the do-or-die part of the case, because the face doesn’t have any blood supply and the clock has been ticking,” Dr. Papay continues. “With every hour that passes, the risk increases that the face could end up permanently not vascularized.
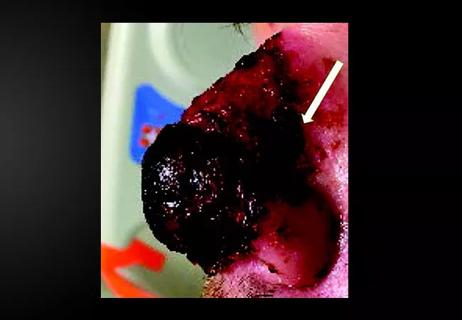
“So we had this face that was very pale and looked cadaveric,” he continues, “and we unclamped the vessels to see if the blood from the recipient would actually flow through all the vessels we had hooked up. There was a hush in the room, and then we all saw this red flush in the face and it lit up like a red light bulb. There was a giant sigh of relief all around. I would say that was the biggest moment and probably the crux of the case.”
His colleague Dr. Gastman concurs. “It was amazing just how much blood flowed into that amount of tissue,” he says. “It was far more than anything I had ever observed in the many facial reconstructions I’ve performed. And that makes sense, because you would never connect an internal jugular vein to an internal jugular vein in a facial reconstruction, yet that’s what we did on one side in this transplant. That’s a gigantic volume of blood flow. The blood itself must have weighed a few pounds.”
Advertisement
“It was a big milestone in the procedure,” says Dr. Papay. “We were all able to relax a bit from that point on.”
Advertisement
Advertisement

Family history may eclipse sun exposure in some cases

Consider secondary syphilis in the differential of annular lesions

Persistent rectal pain leads to diffuse pustules

Two cases — both tremendously different in their level of complexity — illustrate the core principles of nasal reconstruction
Stress and immunosuppression can trigger reactivation of latent virus

Low-dose, monitored prescription therapy demonstrates success

Antioxidants, barrier-enhancing agents can improve thinning hair