Review shows that the disease isn’t only in young women with obesity
Idiopathic intracranial hypertension (IIH) is a rare, vision-threatening disorder, thought to affect predominantly women who are overweight or have obesity. Fulminant IIH is an even rarer subset of the disease and can cause rapid, permanent blindness. Patients often present with headaches and vision changes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
While the prevalence of fulminant IIH more than doubled between 2002 and 2016, presumably due to the increasing prevalence of obesity, research on the condition remains thin. The landmark study on fulminant IIH, published in 2007, was comprised of only 16 women.
“Within this small cohort, 50% remained legally blind,” says Devon Cohen, MD, a neuro-ophthalmologist at Cleveland Clinic Cole Eye Institute. “Clearly, there’s a dearth of research on this condition that can cause severe, irreversible vision loss if not recognized and promptly treated.”
IIH accounts for approximately one-third of Dr. Cohen’s medical practice, she estimates, noting that the volume increased following the COVID-19 pandemic. Multiple case reports have suggested an association between COVID-19 infection and intracranial hypertension.
To help develop a more thorough understanding and accurate characterization of fulminant IIH, Dr. Cohen and a Cleveland Clinic research team recently conducted a literature review of 36 case studies and case series involving 72 patients.
“Our findings add new details to the conventional understanding of the disease,” Dr. Cohen says. “They may change how ophthalmologists and other providers clinically address patients presenting with symptoms, some of whom may have been overlooked in the past.”
According to the 2007 study, 100% of patients with fulminant IIH were women (mean age 23.8) with obesity, headache and severe vision loss. According to Cleveland Clinic’s 2024 review, of the 72 patients with fulminant IIH:
Advertisement
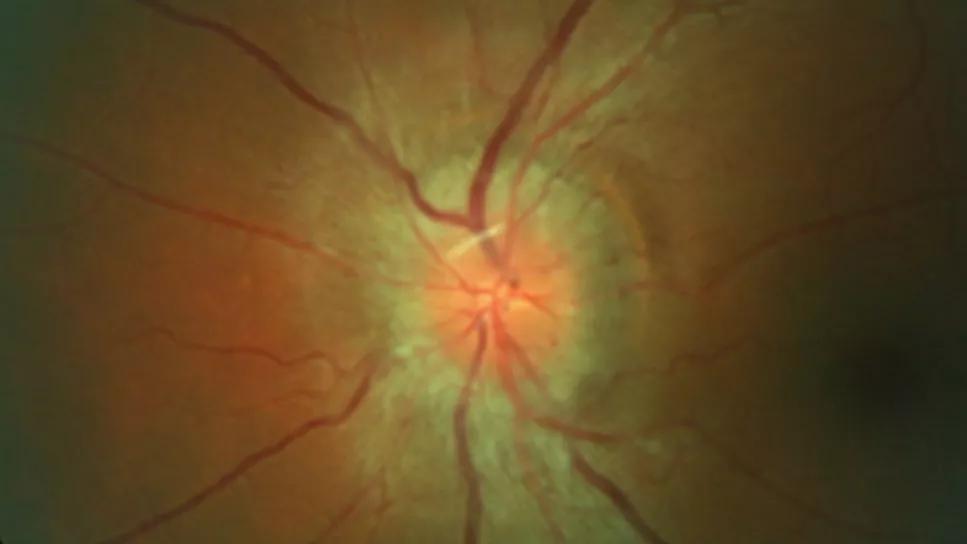
Headache, pulsatile tinnitus and vision changes can be symptoms of intracranial hypertension. When a patient presents with these symptoms, Dr. Cohen recommends a comprehensive ophthalmic exam including a visual field test. Remember: Some patients may be 20/20 on visual acuity testing yet have peripheral vision loss.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a844926e-0130-4c18-8a4d-98961be28f1a/Fulminant-idiopathic-intracranial-hypertension-causing-vision-loss-inset)
In a patient with 20/20 visual acuity, visual field testing shows vision loss, and fundus photography shows profound optic disc edema.
“Accurate and efficient diagnosis can have a profound impact on the patient’s quality of life,” she says. “The right treatment at the right time can preserve vision. In fulminant IIH, we have only a small window before devastating vision loss can occur.”
When Dr. Cohen diagnoses fulminant IIH, she hospitalizes the patient for an immediate workup (including lumbar puncture to measure the pressure of cerebrospinal fluid) and quick initiation of temporizing measures, such as acetazolamide, lumbar drains and consideration of surgical intervention.
Optic nerve sheath fenestration (36% of patients in Cleveland Clinic’s review) is a common procedure. Lumboperitoneal and ventriculoperitoneal shunting are other options (25% and 14%, respectively). Dr. Cohen favors venous sinus stenting (13%) in the appropriate clinical context, given the overall positive outcomes seen at Cleveland Clinic, with fewer significant complications than with shunting.
In pediatric patients, Dr. Cohen advises watching for sixth cranial nerve palsy (abducens nerve palsy). This finding occurred in nearly 86% of pediatric cases of fulminant IIH in Cleveland Clinic’s review.
When pediatric patients present with this palsy, they should have a comprehensive dilated eye exam to evaluate for optic disc edema.
Advertisement
“Fulminant IIH affects a small — yet growing — fraction of the population, but its impact on those patients’ vision and quality of life is significant,” Dr. Cohen says. “More collaborative research is needed to advance treatment.”
Advertisement
Advertisement

For patients with headache, pulsatile tinnitus or vision changes, immediately stop use and refer to ophthalmology

Sustained weight loss helps reduce IIH symptoms and medication dependence

Motion-tracking Brillouin microscopy pinpoints corneal weakness in the anterior stroma

Registry data highlight visual gains in patients with legal blindness

Prescribing eye drops is complicated by unknown risk of fetotoxicity and lack of clinical evidence

A look at emerging technology shaping retina surgery

A primer on MIGS methods and devices

7 keys to success for comprehensive ophthalmologists