A case study with Rula Hajj-Ali, MD
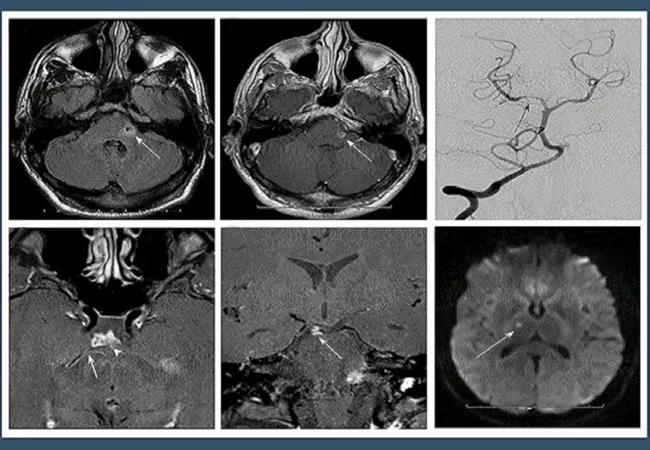
A 32-year-old male presented to the emergency department with left facial numbness/drooping, dizziness and double vision. He has a history of chronic migraine since adolescence, and reports that they have been worsening in the last 6 months. He also has a several-month history of episodic dizziness with associated diplopia and left facial numbness/weakness for the past 6 months. Five months prior to presentation, the patient had been evaluated at another hospital system. Brain MRI at that time revealed a small infarct, for which he was treated with aspirin.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Brain MRI on admission to Cleveland Clinic revealed a new subacute left cerebellar infarct. Watch the video below, with Rula Hajj-Al, MD, to find out the next step in the differential diagnosis.
Video content: This video is available to watch online.
View video online (https://www.youtube.com/embed/bqpVRTt3Pwc?feature=oembed)
Is it CNS Vasculitis?
Although several tools are available to assist in the diagnosis of central nervous system vasculitis (CNS-V), many challenges remain in critically assessing their diagnostic sensitivity and specificity. Diagnostic studies include routine laboratory testing, cerebrospinal fluid assessment, neuroimaging studies, cerebral angiography and biopsy of CNS tissues. Screening laboratory studies performed on blood have little positive predictive value. Also, the specificity of these tests is too low to secure a diagnosis. Various tests for chemistries and autoantibodies as well as cultures and other investigations are useful for ruling out infectious, systemic inflammatory diseases and other hereditary syndromes. Timely diagnosis is extremely important to ensure accurate treatment before irreversible brain damage occurs. Few clinicians are highly experienced with this disease. The care and diagnosis of patients with CNS-V require a team of experts who are familiar not only with this disease but also with its mimics to ensure an accurate diagnosis and workup.
Advertisement
Advertisement

The case for continued vigilance, counseling and antivirals

High fevers, diffuse rashes pointed to an unexpected diagnosis

No-cost learning and CME credit are part of this webcast series

Summit broadens understanding of new therapies and disease management

Program empowers users with PsA to take charge of their mental well being

Nitric oxide plays a key role in vascular physiology

CAR T-cell therapy may offer reason for optimism that those with SLE can experience improvement in quality of life.

Unraveling the TNFA receptor 2/dendritic cell axis