Study finds significant histologic differences between TNFi-induced psoriasis and idiopathic psoriasis

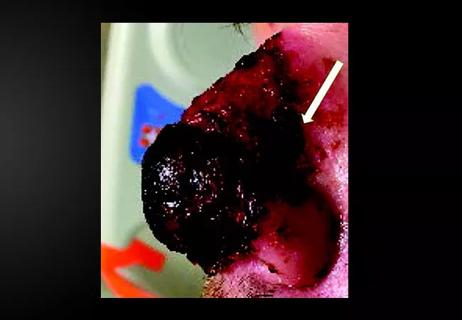
Eosinophils are frequently present in the dermis — and often in higher numbers — in anti-tumor necrosis-factor inhibitor (TNFi)- induced psoriasis compared to idiopathic psoriasis, a new study finds. Distinguishing between these conditions is important when deciding how to treat the psoriasis, and whether or not to continue TNFi treatment for the underlying disease.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The study, which was conducted by a group of Cleveland Clinic investigators found that several histologic parameters were significantly different in TNFi-induced psoriasis biopsy specimens compared to idiopathic psoriasis specimens. Study findings — the first to compare and report histological differences between these two types of psoriatic lesions — were published online by the Journal of the American Academy of Dermatology in January 2020.
“The most important histological differentiator that we found was the presence of eosinophils in the dermis [in the specimens of patients with TNFi-induced psoriasis],” says Cleveland Clinic dermatologist and dermatopathologist, Anthony P. Fernandez, MD, PhD, the study’s corresponding author. “We have done a previous study to show that eosinophils are very rarely found in biopsies of idiopathic psoriasis, whereas we found that they were frequently present and often present in higher numbers in TNFi-induced psoriasis.”
Dr. Fernandez explains that the main goal of the study was to find a test capable of distinguishing between idiopathic psoriasis and TNFi-induced psoriasis, because, clinically, these lesions look the same.
“We believe that the psoriasis that occurs in a lot of patients who are taking TNFis really represents a drug reaction — a rash that is precipitated by medication,” he says. He notes that many patients taking TNFis already have an underlying higher risk of developing psoriasis. “So, what we want to know is, whether these patients who are taking TNFis have naturally developed psoriasis or is it the medication that is causing it?”
Advertisement
Distinguishing between idiopathic and TNFi-induced psoriasis can have significant implications on the management of patients whose underlying inflammatory conditions are controlled by the medication, such as inflammatory bowel disease, psoriatic arthritis or rheumatoid arthritis.
“When patients develop a moderate or severe psoriatic reaction, we do not want the clinician’s knee-jerk reaction to be removal of the TNFi,” he says. “If the TNFi is working well for the other condition, we want to do everything we can to keep the patients on it.”
Dr. Fernandez explains that his earlier study, published in the Journal of the American Academy of Dermatology, found that TNFi-induced psoriasis can usually be effectively controlled with topical or systemic medications.
“We found [in our published cohort] that we could control the majority of patients by just adding topical medications, creams or ointments alone,” he says. “When those were not effective, we could often add oral medications, either methotrexate or cyclosporine, and that would then control the reaction.”
The present study characterized 60 biopsy specimens obtained from 47 patients who developed TNFi-induced psoriasis and were treated at Cleveland Clinic between 2004 and 2016. The histologic features of those specimens were compared to those of 85 control biopsy specimens obtained from a group of 85 patients with idiopathic psoriasis. The histologic reaction pattern was most commonly Psoriasiform (80%); five histologic parameters were significantly different in TNFi-induced psoriasis specimens.
Advertisement
“We found that if patients had at least three eosinophils in a single histologic section under the microscope, then this was a very strong predictor of TNFi-induced psoriasis and not idiopathic psoriasis,” says Dr. Fernandez. Neutrophils in the stratum corneum and papillary plate thinning were more significantly likely in typical (or idiopathic) psoriasis, whereas neutrophils in the epidermis and lack of parakeratosis was more significantly seen in TNFi-psoriasis. The study did not find a clear relationship between a specific TNFi and TNFi-induced psoriasis.
“We do not think that different TNFis are necessarily associated with an increased risk of psoriasis compared to others,” says Dr. Fernandez. “I suspect that there is some other trigger, just like we think that there is for typical psoriasis or psoriatic arthritis. The question is: What is that trigger?”
One thing that seems to correlate with the development of TNFi-induced psoriasis is a family history of psoriasis, explains Dr. Fernandez. “There may be some genetic component, which, in the right setting of TNF blockade, can precipitate this reaction.”
The ongoing research efforts of Dr. Fernandez’s team are focused on identifying the risk factors and triggers of TNFi-induced psoriasis. Knowing the predictors and risk factors could help improve our confidence in diagnosing TNFi-psoriasis and potentially even impact our decision-making process when considering TNFis versus other medications for patients.
“We are looking at our cohort of patients with TNFi-induced psoriasis and a group of control patients of similar age, sex, underlying disease and treatment with TNFi to see if we can identify any precipitating effects or risk factors of TNFi-psoriasis,” he says. “We’re in the data analysis stage of this project and we believe we will soon have some interesting findings to share.”
Advertisement
Advertisement

Family history may eclipse sun exposure in some cases

Consider secondary syphilis in the differential of annular lesions

Persistent rectal pain leads to diffuse pustules

Two cases — both tremendously different in their level of complexity — illustrate the core principles of nasal reconstruction
Stress and immunosuppression can trigger reactivation of latent virus

Low-dose, monitored prescription therapy demonstrates success

Antioxidants, barrier-enhancing agents can improve thinning hair