PARTNER 2 analysis finds few significant effects

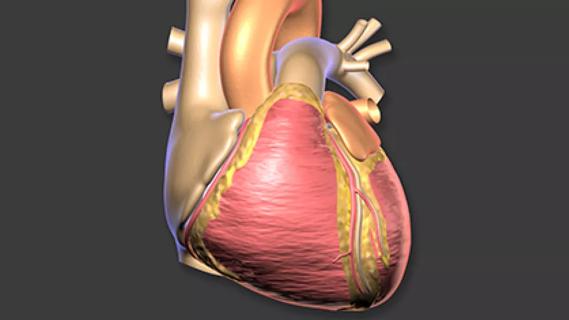
An analysis of PARTNER 2 trial and registry data found that anticoagulation therapy had no significant short-term impact on valve hemodynamics and most clinical outcomes in both transcatheter and surgical bioprosthetic aortic valve replacement (AVR), but anticoagulation reduced short-term risk of stroke after surgical AVR (SAVR). The results were published by a team of PARTNER 2 investigators in the Journal of the American College of Cardiology (2019;74:1190-1200).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In 2017, the American College of Cardiology/American Heart Association issued a guideline update recommending three months of anticoagulation therapy for AVR patients at low risk of bleeding, regardless of replacement method. The recommendation was a controversial answer to an unsettled question.
“The idea was that thrombus could form on the valve before complete endothelialization or that short-term anticoagulation could decrease the risk of thromboembolism from unrecognized new-onset atrial fibrillation,” says Cleveland Clinic Cardiovascular Medicine Chair Samir Kapadia, MD, a PARTNER 2 investigator and co-author of the new analysis. “This makes sense but was not supported by evidence that antithrombotic and antiplatelet therapies make a difference in patients with bioprosthetic valve replacement. This analysis moves us toward more evidence-based practice.”
The study pooled data from 4,832 patients undergoing bioprosthetic AVR in the PARTNER 2 randomized trials and nonrandomized registries (transcatheter AVR [TAVR], n = 3,889; SAVR, n = 943). The researchers collected data on anticoagulation therapy at discharge — defined as antiplatelet and/or antithrombotic therapy — as well as 30-day and one-year post-AVR echocardiograms. They used a linear regression model to assess the impact of anticoagulation on valve hemodynamics and a Cox proportional model with propensity-score adjustment to measure any effect on clinical outcomes.
Across the overall study sample, about one-third of patients received anticoagulation therapy at discharge — 29.2% of the TAVR cohort and 36.3% of the SAVR cohort.
Advertisement
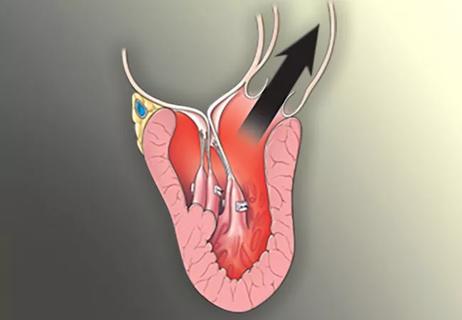
After adjusting for annular diameter, atrial fibrillation, valve size and ejection fraction at the time of hemodynamic assessment, the researchers found that discharge on anticoagulation didn’t significantly impact aortic valve mean gradients or aortic valve areas in either the TAVR or SAVR cohorts. At the same time, a significantly smaller proportion of patients discharged on anticoagulation experienced a rise in mean gradients of >10 mm Hg compared with those not discharged on anticoagulation (1.3% vs. 2.3%; P = 0.03). “Whether this early benefit of preventing valve deterioration amounts to long-term benefit in valve durability remains unknown,” notes Dr. Kapadia.
In terms of clinical outcomes, anticoagulation was not independently associated with rates of death, rehospitalization, myocardial infarction, prosthetic valve dysfunction or aortic valve reintervention in either the TAVR or SAVR cohorts. Analysis did, however, reveal a link between anticoagulation therapy and reduced risk of stroke among patients undergoing SAVR (hazard ratio [HR] = 0.17; 95% CI, 0.05-0.60; P = 0.006).
“Although speculative, this potentially points to the theory of benefit from unrecognized new-onset atrial fibrillation in the SAVR population,” observes Dr. Kapadia. “That said, the absolute risk of stroke is very low, so it remains controversial whether this justifies routine anticoagulation or not.”
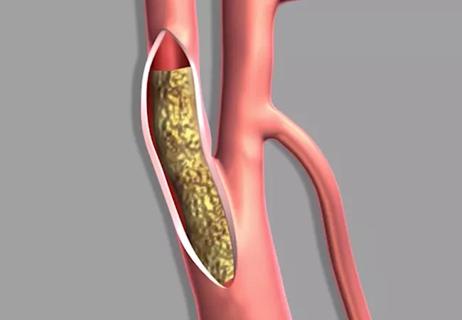
Anticoagulation did not make a difference in major or life-threatening bleeding, but TAVR patients discharged on anticoagulation had an increased rate of minor bleeding (HR = 1.72; 95% CI, 1.13-2.61; P = 0.01).
Advertisement
As use of bioprosthetic valves increases in both TAVR and SAVR, the lack of adverse effects from anticoagulation therapy in this study is reassuring. But the authors note that limitations of their study — including short-term follow-up, lack of post-AVR CT imaging, and lack of assessment of specific antiplatelet and antithrombotic regimens — temper the results.
“Until we see the detailed results from ongoing randomized controlled trials,” says Dr. Kapadia, “clinicians should assess and advise patients on an individualized basis as to the best postoperative management strategy to reduce short-term thrombus risk after bioprosthetic valve implantation. This should include clear discussion about a potentially increased risk of minor bleeding with anticoagulation after TAVR and a potentially decreased risk of stroke after SAVR.”
He notes that several issues are highly pertinent in the context of such discussions and related decision-making:
Advertisement
Advertisement

Study authors urge reevaluation of the sweetener’s safety designation by food regulators

Surprise findings argue for caution about testosterone use in men at risk for fracture

Findings support emphasis on markers of frailty related to, but not dependent on, age
![GettyImages-1252287413 [Converted]](https://assets.clevelandclinic.org/transform/StoryPanel/350804b2-f1e4-4d97-a277-9629cf45af3e/23-HVI-4120348_redlining_650x450_jpg?w=3840&q=75)
Large database study reveals lingering health consequences of decades-old discrimination
Additional analyses of the two trials presented at 2023 ESC Congress
Prospective SPIRIT-HCM trial demonstrates broad gains over 12-month follow-up

An ACC committee issues recommendations to accelerate sluggish progress
Review of our recent experience shows it’s still a safe option