A review of our approach

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/41c5a1f7-26c1-4839-9c0c-8b28a89aea7b/Twitter-170116-16-NEU-1945-Walia-650x450-478297788_jpg)
Twitter-170116-16-NEU-1945-Walia-650×450-478297788
By Loutfi S. Aboussouan, MD, FCCP, and Eduardo Mireles-Cabodevila, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
More than 40 percent of patients with neuromuscular disease suffer from sleep-disordered breathing events. The more advanced the disorder, the higher the prevalence of sleep-related breathing issues from common neuromuscular disease features like anatomic or neurologic propensity to obstructive sleep apnea, potential cardiomyopathy and diaphragmatic weakness.
In a recent review in CHEST, we discuss common pathophysiology we see in our neuromuscular diseases clinic, which incorporates expert physicians from Cleveland Clinic’s Sleep Disorders Center, Respiratory Institute and Neurological Institute as well as experienced respiratory and physical therapists.
Patients with neuromuscular disease often exhibit varying degrees of restrictive physiology on pulmonary function testing. Lung restriction typically begins early in the disease course with a decrease in vital and inspiratory capacities. Further reduction of the vital capacity in the supine position and a decrease in chest wall compliance contribute to this restrictive physiology.
Respiration is particularly vulnerable during sleep when lung volumes are further reduced due to the combined effects of the neuromuscular disease, the supine position and the physiologic processes of sleep itself. Patients with neuromuscular disease are more vulnerable to the normal loss of inspiratory intercostal muscle tone during rapid eye movement (REM) sleep. Reduced chemosensitivity and reduced activity of pharyngeal dilators during sleep also compromise respiration during REM sleep.
Advertisement
A variety of sleep-disordered conditions are associated with the various neuromuscular diseases. These are highlighted in the table below, along with the mechanisms responsible for the development of these complications. The table is intended to be representative rather than exhaustive.
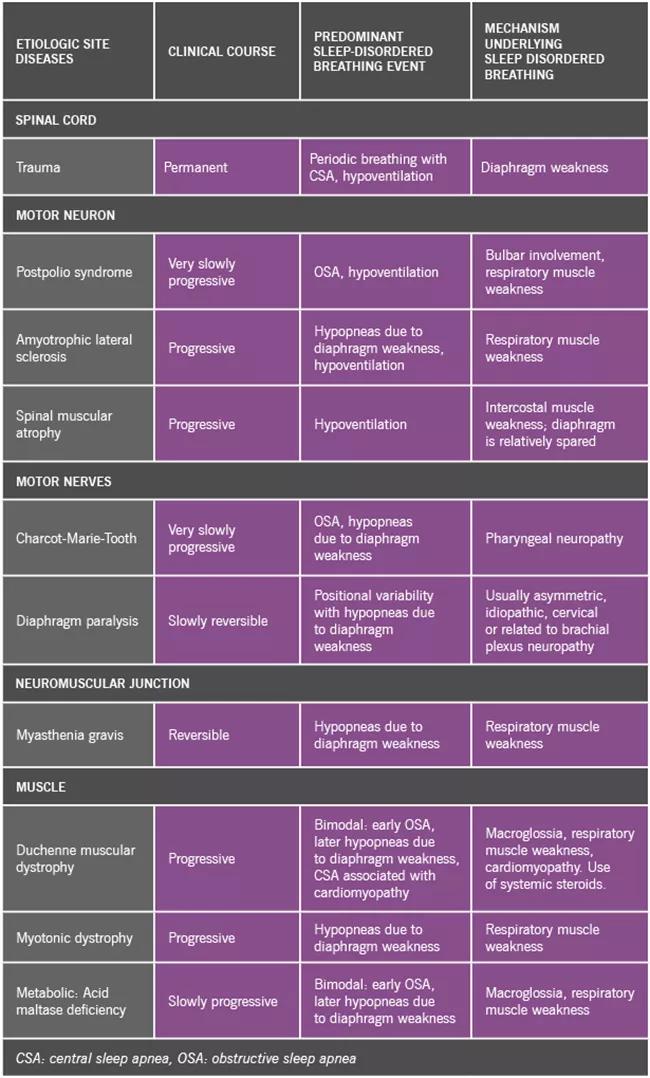
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/16855ed0-2b85-4783-b3a9-11e18d874483/17-PUL-259-Aboussouan_ConsultQD_Inset-Table_jpg)
Types of sleep-disordered breathing in representative neuromuscular conditions categorized by site of disease.
We use a specific protocol to analyze patients with neuromuscular disease who undergo a sleep study. Our hypoventilation protocol includes transcutaneous monitoring of carbon dioxide levels and is specifically designed to address both obstructive events and hypoventilation.
We also work to reduce treatment burden on our patients. Many of our patients, especially those with amyotrophic lateral sclerosis (ALS), face multiple therapies and appointments. Accordingly, our neuromuscular clinic coordinates with the multidisciplinary ALS/motor neuron disease clinic of the Neuromuscular Center so that visits with physiatrists, social workers, therapists, neuromuscular and pulmonary physicians and pulmonary function testing are accomplished in a single day.
Our clinic specializes in providing all modalities of invasive and noninvasive ventilation. We use noninvasive mechanical ventilation and tailor the therapy to the patient’s needs. Our aim is to maintain patient autonomy and allow mobility, travel and speech. We also use various interfaces (oral, nasal, full face masks) and modes (volume- or pressure-controlled modes, including some automatic algorithms like Average Volume Assured Pressure Support [AVAPS]). We evaluate adherence and adjust the settings based on clinical signs, measurement of end tidal CO2 and nocturnal pulse oximetry. We use polysomnography to adjust settings in patients with complex issues. We monitor our patients carefully in the context of bulbar and cardiac dysfunction.
Advertisement
In addition to sleep-related respiratory issues, our clinic focuses on secretion management and airway clearance. Much of the morbidity of neuromuscular diseases is related to the buildup of secretions and difficulties in their management. Options include control of secretions at their source (such as nasal spray), use of mucolytic agents that may reduce their viscosity (including nebulized treatments) and mechanical options that may facilitate their clearance (such as oscillatory valves or vest and cough-assist devices).
For a more in-depth discussion of sleep disorders associated with neuromuscular disease, their polysomnographic features, and treatment, read our full review in CHEST.
Dr. Aboussouan is staff in the Respiratory and Neurological Institutes and the Sleep Disorders Center. Dr. Mireles-Cabodevila is staff in the Respiratory Institute.
Advertisement
Advertisement
The disease’s neuropathologic heterogeneity holds clues to refining diagnosis and prognosis
A case study in pairing imaging acumen with subspecialty expertise to yield answers and symptom relief
Guidance from the largest cohort of SEEG-confirmed insular epilepsy patients reported to date
Ethical guidance provides guardrails so medical advances benefit patients
OCEANIC-STROKE results represent long-sought advance in secondary stroke prevention
Two studies from Cleveland Clinic may help advance the technology toward broader clinical use
Distinct MRI signature includes lesions beyond the corpus callosum, features predictive of vision and hearing loss
An argument for clarifying the nomenclature