What have we learned?
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
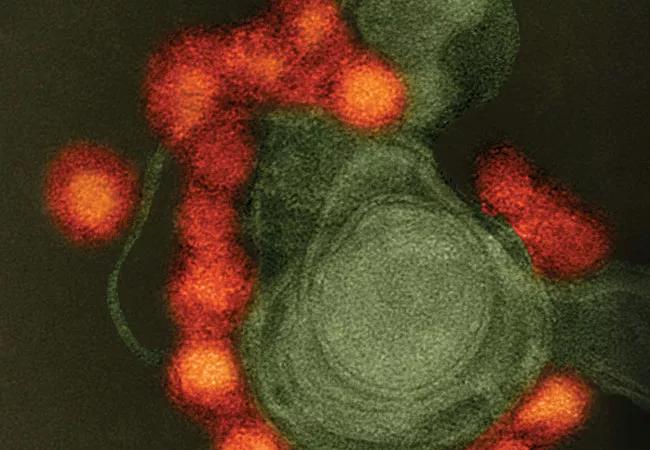
In late summer of 2016 I wrote an article entitled, RA or Chikungunya? The Rheumatologist’s Primer on Tropical Mosquito-Related Viruses. We’ve learned quite a bit about the virus in the few short months since the article was published. As of August 2016, every country in North, Central and South America (with the exceptions of Canada and Chile) has reported active Zika transmission. Every U.S. state has been affected except Alaska.
Zika represents a disorder that can produce a wide array of rheumatic symptoms in patients. For any patients presenting with a febrile syndrome including inflammatory polyarthritis, rash, conjunctivitis, myalgia and headache, ask them:
1) Have you been in an area in which Zika is prevalent?
Zika should be considered a possible diagnosis primarily in patients returning from the tropics (including U.S. territories such as Puerto Rico, the U.S. Virgin Islands and American Samoa) but also for any individual who has been to areas where Anopheles mosquitoes are carrying the virus, such as South Florida.
2) Have you been in sexual contact with a person who might have Zika?
Zika has now been conclusively documented to be sexually transmitted from man to woman and woman to man and can be so transmitted for at least two months following infection.
If the answer to either question is yes, keep Zika infection within your differential diagnosis.
Our knowledge of this virus is constantly evolving; to stay current, subscribe to the Zika Reporter Bulletin, an independent and free recurring summary of Zika updates (zikareporter.com).
Advertisement
Dr. Calabrese is Director of the R.J. Fasenmyer Center for Clinical Immunology in the Department of Rheumatic and Immunologic Diseases.
Advertisement
Advertisement

The case for continued vigilance, counseling and antivirals

High fevers, diffuse rashes pointed to an unexpected diagnosis

No-cost learning and CME credit are part of this webcast series

Summit broadens understanding of new therapies and disease management

Program empowers users with PsA to take charge of their mental well being

Nitric oxide plays a key role in vascular physiology

CAR T-cell therapy may offer reason for optimism that those with SLE can experience improvement in quality of life.

Unraveling the TNFA receptor 2/dendritic cell axis