Management options expand in both inpatient and outpatient settings
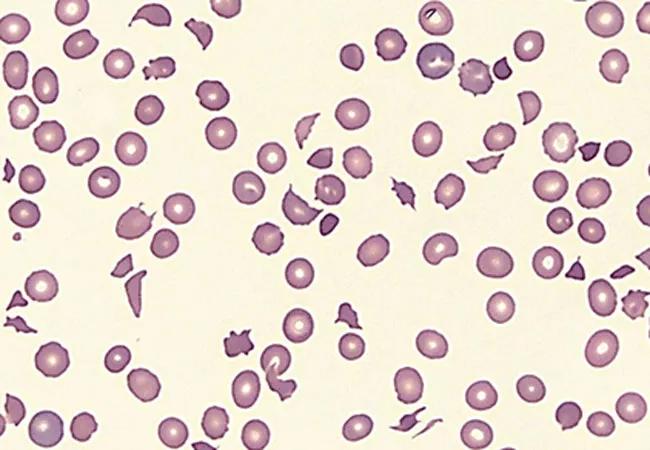
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/f721365c-542d-46b1-b6ef-1551ecb0880d/rogers_adamts13_650x450-jpg)
Blood cells
The American Society of Hematology (ASH) guidelines for the management of patients with immune thrombocytopenic purpura (ITP) have been updated to focus on treating patients without bleeding in both outpatient and inpatient settings, including those with newly diagnosed, persistent, and chronic ITP refractory to first-line therapy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Current recommendations for therapy — an update to the organization’s 2011 guidelines — include corticosteroids, intravenous immunoglobulins, anti-D immunoglobulin, rituximab, splenectomy, and thrombopoietin-receptor agonists, as well as observation.
Published in 2019, the revised guidelines can help practitioners decide on inpatient vs. outpatient management, thresholds for initiating treatment, and options for second-line therapy in adults, explains Dana Angelini, MD, hematologist and medical oncologist in Cleveland Clinic’s Taussig Cancer Institute.
Inpatient management is suggested for those with newly diagnosed ITP who have a platelet count below 20 × 109/L and are asymptomatic or have minor symptoms, including wet purpura, gum bleeding, continuous epistaxis needing intervention, menorrhagia, or multiple large (≥3 m) bruises.
Outpatient management can be considered for patients with a platelet count of at least 20 × 109/L who are asymptomatic or have minor mucocutaneous bleeding (e.g., few petechiae, bruises <3 cm, or epistaxis on nose-blowing). It can also be considered for patients with established ITP who have a platelet count below 20 × 109/L and are asymptomatic or have minor symptoms. Asymptomatic patients or those with a documented good response to rescue agents can be followed as outpatients.
Observation can be considered for newly diagnosed patients with a platelet count of at least 30 × 109/L who are asymptomatic or have minor mucocutaneous bleeding. The updated guidelines note the need for clinical judgment for patients who have additional comorbidities, are scheduled for procedures, or have more than minor bleeding. It is important to consider concomitant medications such as anticoagulant and antiplatelet drugs, as higher platelet thresholds are more desirable in this setting. Patients with a history of bleeding also warrant consideration for a higher platelet goal and may warrant treatment rather than observation.
Advertisement
Corticosteroid therapy should be considered for newly diagnosed patients with a platelet count less than 30 × 109/L who are asymptomatic or patients with minor or more significant bleeding. The presence of severe thrombocytopenia also warrants consideration for a more aggressive approach, such as a combination of high-dose steroids and other rescue agents (e.g., IV immunoglobulins or anti-D immune globulins). Steroid therapy warrants extra consideration in patients with poorly controlled diabetes and those who are immunocompromised.
Regarding the type and duration of steroids, the guidelines recommend against a long course of prednisone (>6 weeks, including taper) in favor of a shorter course (≤6 weeks). When considering dexamethasone vs. prednisone, either is acceptable (prednisone 0.5–2.0 mg/kg/day or dexamethasone 40 mg/day for 4 days). However, if a rapid response is desired, dexamethasone is preferred. Of note, there appears to be no benefit with regard to response at 1 month, durability of response, or major bleeding between these treatment options.
In addition, the guidelines suggest using corticosteroids alone for initial treatment rather than in combination with rituximab as first-line therapy.
The guidelines provide recommendations on managing adults with ITP who are corticosteroid- dependent or unresponsive to corticosteroids. Of note, corticosteroid dependence has been defined as an ongoing need for continuous prednisone at more than 5 mg/day (or corticosteroid equivalent) or as requiring frequent courses of corticosteroids to maintain a platelet count of at least 30 × 109/L or to avoid bleeding.
Advertisement
The updated guidelines are based on retrospective and indirect comparisons. In practice, the recommendations for second-line therapy are based on shared decision-making after a review of risks and benefits and patient preferences.
When choosing a second-line therapy in adults with ITP lasting 3 months or longer, the guidelines suggest the following:
When choosing between a TPO-RA, splenectomy, or rituximab for a second-line therapy, practitioners are encouraged to use shared decision-making, taking into account patient preferences with regard to potential complications, side effects, and treatment duration, along with the following:
Advertisement
Dr. Angelini adds that it should be noted that no clinical trials have directly compared the TPO-RAs eltrombopag and romiplostim. Guidelines suggest either one agent or the other, noting that individual patients may place a higher value on a daily oral medication vs. weekly subcutaneous injection.
Of note, these guidelines do not mention avatrombopag as a potential second-line agent. Avatrombopag is a TPO-RA approved by the US Food and Drug Administration (FDA) in 2019 for treating thrombocytopenia in patients with chronic ITP who have had an insufficient response to previous therapy.
Avatrombopag is now considered an option for second-line therapy based on its FDA approval as well as safety and efficacy data showing that it is an effective option for patients with ITP who have had an insufficient response to the initial treatment regimen.
Eltrombopag is considered more cost-effective than romiplostim. Oral administration (eltrombopag and avatrombopag) vs. subcutaneous injection (romiplostim) along with food interactions (with eltrombopag) should be discussed with the patient.
For patients with a predictable response to rescue therapy, the updated ASH guidelines will help reduce hospital admissions for those with asymptomatic ITP with severe thrombocytopenia, explains Dr. Angelini. The advantages and disadvantages of available second-line therapies are briefly discussed to inform shared decision-making with patients. The guidelines stress the importance of monitoring for side effects of glucocorticoid therapy and highlight pre- and postsplenectomy vaccination care.
Advertisement
With multiple drugs approved for ITP management in the last decade, the updated guidelines aim to stratify the sequence of use of the newer drugs to minimize cost, side effects, and long-term complications.
Although these guidelines address decision-making for patients with symptomatic ITP with severe thrombocytopenia, there is limited guidance about treating asymptomatic patients whose platelet counts are below 100 × 109/L but over 30 × 109/L. The guidelines are broadly applicable to ITP management and most patient populations. However, they do not specifically comment on pregnant patients, the management of secondary ITP, or treatment options beyond the use of TPO-RA, rituximab, or splenectomy as second-line agents. Fostamatinib, a splenic tyrosine-kinase inhibitor, is an approved ITP therapy but is not specifically discussed in these guidelines, as it has primarily been studied in the third-line setting.
This article originally appeared in the Cleveland Clinic Journal of Medicine and has been abbreviated for Consult QD.
Advertisement
Goal-of-care discussions drive earlier hospice access
Clinical trials and de-escalation strategies
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting