Identifying correct ablation pattern helps select correct IOL calculator
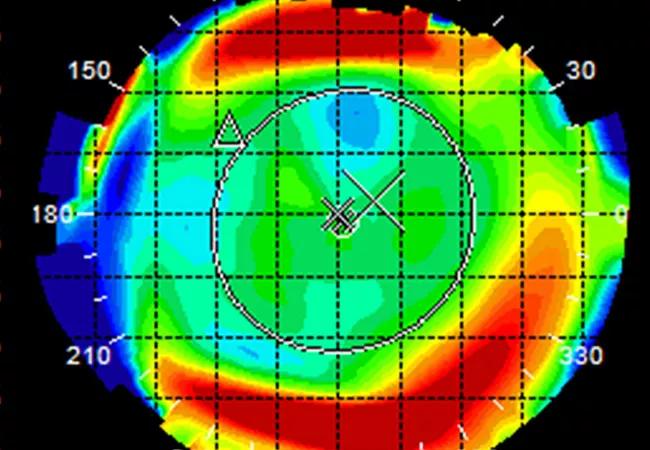
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/220ff200-b765-4646-9de3-5978b8c18fa2/21-EYE-2084160-CQD-Topography-Pattern-Recognition-Analysis_jpg)
21-EYE-2084160-CQD-Topography-Pattern-Recognition-Analysis
By J. Bradley Randleman, MD, and Jeffrey Goshe, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The number of patients with a history of laser in situ keratomileusis (LASIK) now presenting with visually significant cataracts is growing exponentially. What was a rare scenario 20 years ago is commonly encountered today, as millions of patients worldwide have LASIK or similar corneal refractive surgeries each year.
These patients present challenges for intraocular lens (IOL) power calculations because the central curvature altered by refractive surgery is not accounted for in traditional calculation methods, and significant postoperative refractive surprises can arise.
To overcome this, a variety of formulas have been developed for both post-myopic and post-hyperopic ablations. Despite these advances, one key step in the process still can prove challenging: recognizing the type of ablation performed (myopic vs. hyperopic) so the correct calculators can be used.
To determine the type of ablation performed, corneal imaging must be obtained. Although multiple technologies exist to image the cornea, the mainstays for determining anterior corneal curvature are Placido-based topography and Scheimpflug-based tomography. Curvature data can be output as either axial or tangential (instantaneous) displays. Most clinicians and devices use axial curvature as their default. However, in determining the type of ablation performed, tangential curvature displays have a decided advantage.
When viewing tangential curvature maps, the juncture created in the periphery by the tissue ablation zone creates focal patterns that differ dramatically between myopic and hyperopic ablations. Myopic ablation results in a focal peripheral steepening at the edge of the centrally flattened optical zone (Figures 1a, 1b), whereas hyperopic ablation results in a focal peripheral flattening at the edge of the centrally steepened optical zone (Figures 2a, 2b).
Advertisement
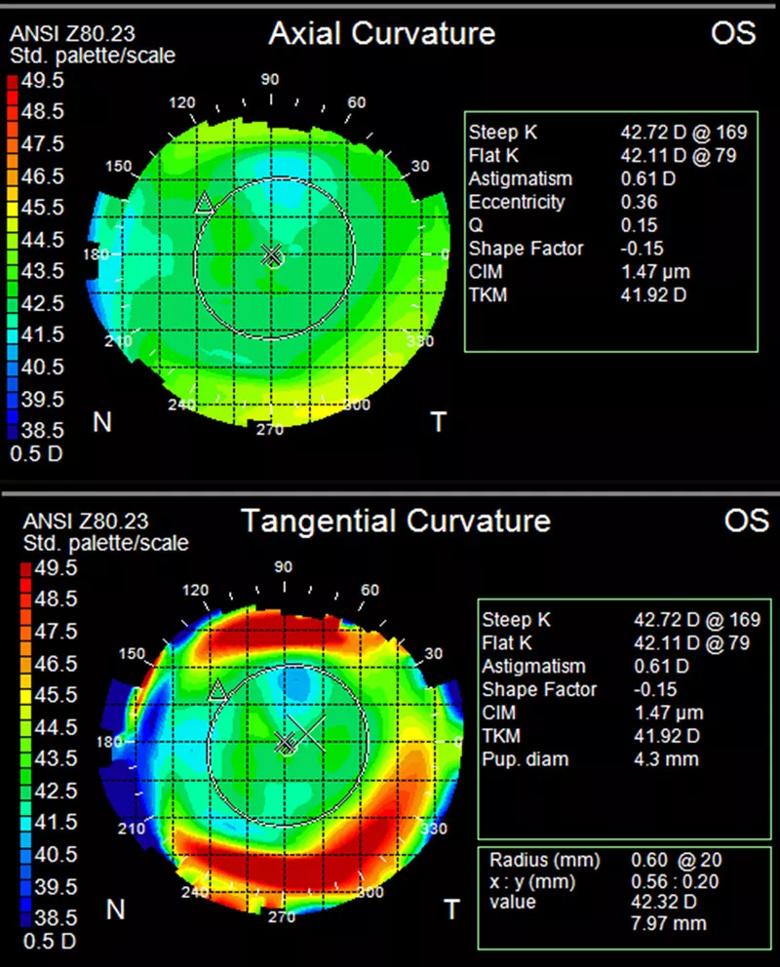
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/1894a7b5-3278-4eec-a9be-6e3cfc562d6a/21-EYE-2084160-Figure-1a-Placido-Myopic-Maps_jpg)
Figure 1a. Placido composite image of the left eye from a patient presenting for cataract evaluation who had a history of undergoing LASIK. In axial maps (upper) the pattern is indistinct, with only a hint of central flattening. In tangential maps (lower), however, the pattern of central flattening with peripheral steepening at the edge of ablation becomes easily discernible, indicating a myopic ablation was performed.
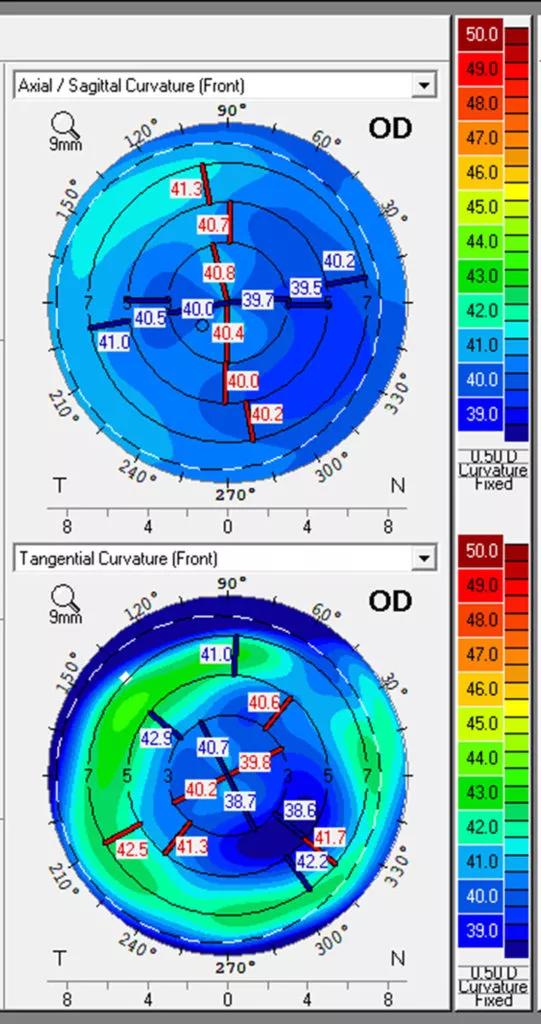
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/9d4cc8c6-b140-4949-a1a9-fa0ceab8763e/21-EYE-2084160-Figure-1b-Scheimpflug-Myopic-Maps-541x1024_jpg)
Figure 1b. Scheimpflug composite image of the right eye from a patient presenting for cataract evaluation who had a history of undergoing LASIK. In axial maps (upper) the pattern is indistinct, with only a hint of central flattening. In tangential maps (lower), however, the pattern of central flattening with peripheral steepening at the edge of ablation becomes easily discernible, indicating a myopic ablation was performed.
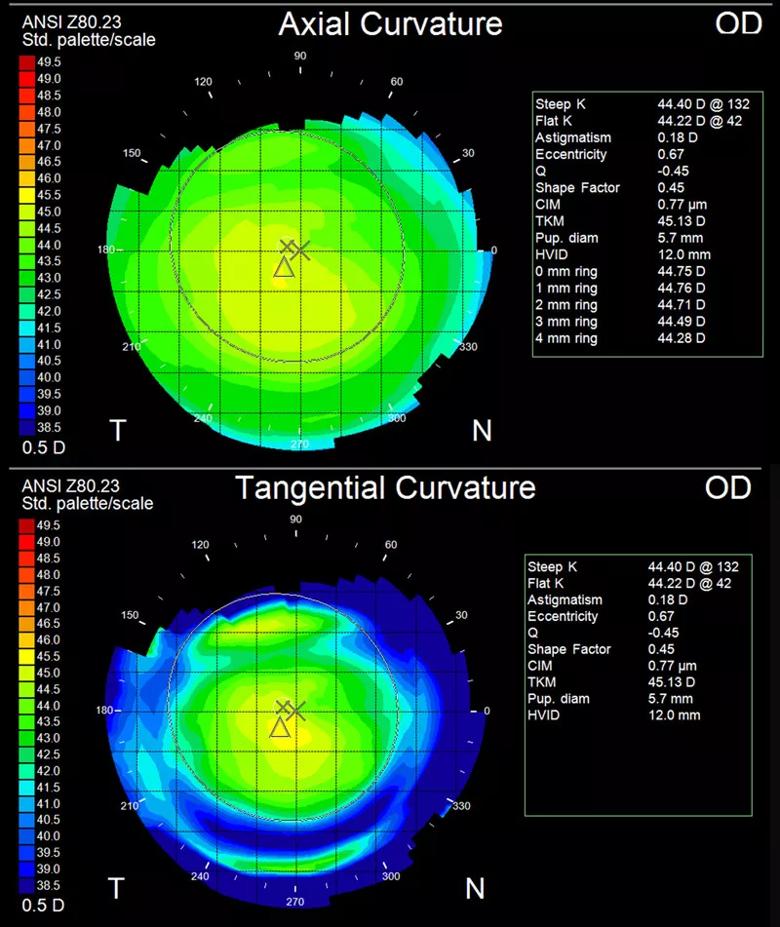
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/cc67fc04-1638-4e4b-8db1-d45908665a6d/21-EYE-2084160-Figure-2a-Placido-Hyperopic-Maps_jpg)
Figure 2a. Placido composite image of the right eye from a patient presenting for cataract evaluation who had a history of undergoing LASIK. In axial maps (upper) the pattern is somewhat unclear, with only a modicum of central steepening apparent. In tangential maps (lower), however, the pattern of central steepening with marked peripheral flattening at the edge of ablation becomes easily discernible, indicating a hyperopic ablation was performed.
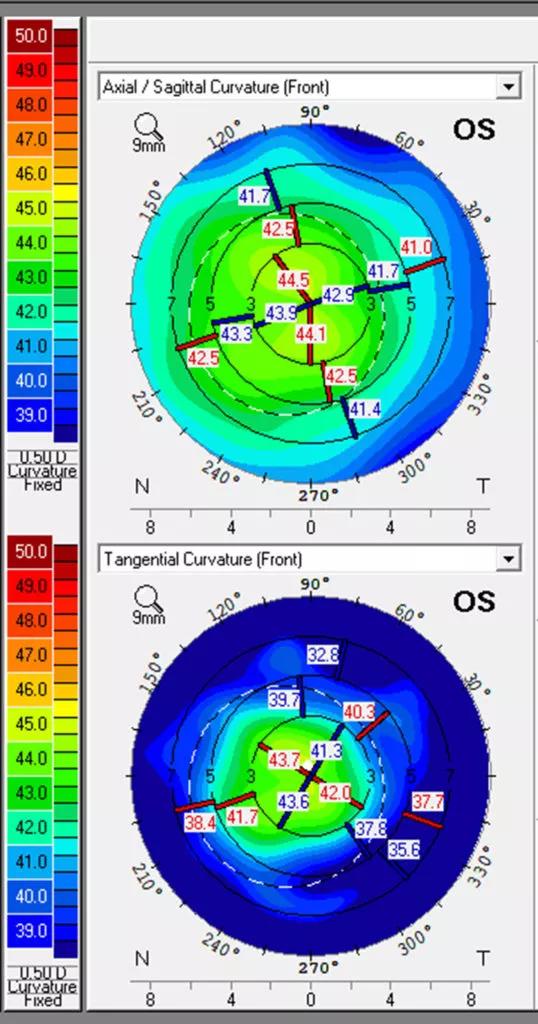
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/381d8b1e-c813-41a3-8c96-16890b382fd8/21-EYE-2084160-Figure-2b-Scheimpflug-Hyperopic-Maps-538x1024_jpg)
Figure 2b. Scheimpflug composite image of the right eye from a patient presenting for cataract evaluation who had a history of undergoing LASIK. Axial maps (upper) show the correction pattern relatively well, with central steepening consistent with hyperopic correction. Tangential maps (lower) more clearly demonstrate the correction pattern, with accentuated central steepening and surrounding flattening better emphasizing the treatment pattern.
Advertisement
To evaluate the use of these curvature displays, we showed a set of corneal images obtained with either Placido-based topography (Zeiss Atlas) or Scheimpflug tomography (Oculus Pentacam®) to ophthalmology residents and cornea fellows at multiple institutions. Results of the study confirmed that these novice reviewers were significantly more likely to correctly identify eyes with myopic or hyperopic ablation patterns using tangential curvature maps (83%-91% correct responses) rather than axial curvature maps (55%-58% correct responses). There was no difference in responses between devices, and no significant differences between residents or fellows in different years of training.
This suggests that greater focus on corneal imaging during training could help future cataract surgeons correctly interpret these maps. As a result of this study, Cole Eye Institute’s residency program now includes dedicated corneal imaging conferences. Educating residents on the various aspects of corneal imaging will be critical to their future practices.
Staff surgeons at Cole Eye Institute were administered the same test, and results were quite similar. The experienced surgeons correctly classified significantly greater numbers of images when they were shown tangential maps.
This resulted in changes to our clinical practice. Our ultrasound team now routinely presents surgeons with both axial and tangential images at the time of IOL calculation and lens selection to confirm that the appropriate calculators and formulas have been used for each post-refractive surgery patient undergoing cataract surgery.
Advertisement
In conclusion, the use of tangential curvature maps significantly improved novice reviewers’ ability to identify previous myopic and hyperopic ablation patterns using both Scheimpflug- and Placido-based imaging technologies. We recommend the use of tangential maps in conjunction with axial curvature maps when evaluating eyes with previous refractive surgery, particularly when the ablation pattern is difficult to identify. This will help cataract surgeons select the correct IOL calculator and, thus, improve IOL power selection for patients with previous refractive surgery.
Dr. Randleman is a specialist in corneal and intraocular refractive surgery at Cole Eye Institute. Dr. Goshe is a specialist in cornea and external disease at Cole Eye Institute.
Advertisement
Advertisement
A review of pathophysiology, risk factors, clinical presentation and treatment options
How computational tools and personalized biomechanics can improve keratoconus detection, ectasia risk assessment and surgical outcomes
Motion-tracking Brillouin microscopy pinpoints corneal weakness in the anterior stroma
Registry data highlight visual gains in patients with legal blindness
Prescribing eye drops is complicated by unknown risk of fetotoxicity and lack of clinical evidence
A look at emerging technology shaping retina surgery
A primer on MIGS methods and devices
7 keys to success for comprehensive ophthalmologists