Aggressive treatment required to control symptoms and prevent central nervous system decline and vision loss
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 28-year-old female living in another state presented to her local retina specialist with a complaint of a blurry spot in the temporal periphery of her right eye. The retina specialist diagnosed her with occlusive retinal vasculitis and put her on an oral prednisone taper. The right eye improved, but she developed symptoms in the left eye after tapering the prednisone. At this time, she was referred to us for evaluation of uveitis.
On presentation to Cole Eye Institute, the patient was noted to have developed other blurry areas in her visual field that would improve after a short time. She stated that all of her testing for causes of uveitis was negative to date. Anterior segment and retinal examinations were normal. An ultra-widefield fluorescein angiogram showed a branch retinal artery occlusion (BRAO) in the left eye (Figure 1). The right eye was normal.
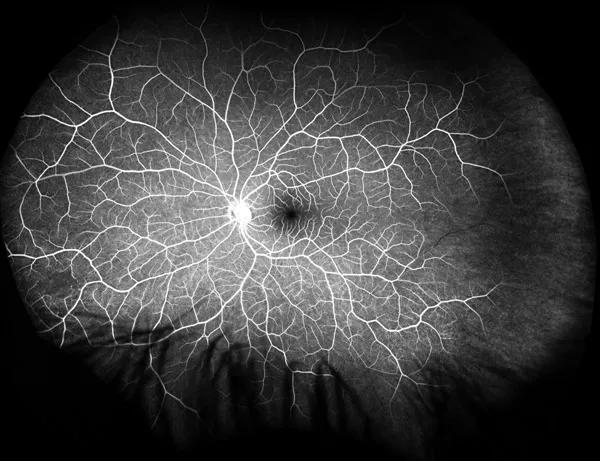
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5b62a9b2-cc46-4af5-bae9-3eb39a27a9c9/17-EYE-1417-Sharma-CQD-Inset-1_jpg)
Figure 1. Ultra-widefield fluorescein angiogram of the left eye at presentation showing a peripheral branch retinal artery occlusion (BRAO) in the temporal periphery and a small area of capillary nonperfusion in the nasal periphery.
On further questioning, the patient admitted to having a few years of progressive hearing loss, progressive irritability (which her husband stated had transitioned to severe mood swings) and progressively worsening headaches. The fluorescein angiographic findings combined with her symptoms led to suspicion for Susac syndrome. We ordered magnetic resonance imaging (MRI) of her brain.
Although the MRI was normal, we decided to proceed with immunosuppression to treat the patient for Susac syndrome. She was started on intravenous immunoglobulin (IVIG), mycophenolate mofetil and pulse IV methylprednisolone.
Advertisement
A few months later, she developed worsening of her headaches. A repeat MRI of her brain showed the characteristic findings of Susac syndrome in the corpus callosum. A fluorescein angiogram (Figure 2) at this time showed reperfusion of the BRAO; however, a new area of vessel wall hyperfluorescence had developed. We stepped up her immunosuppression regimen to include rituximab. Her headaches subsided, and she has not had any further episodes of vision loss.
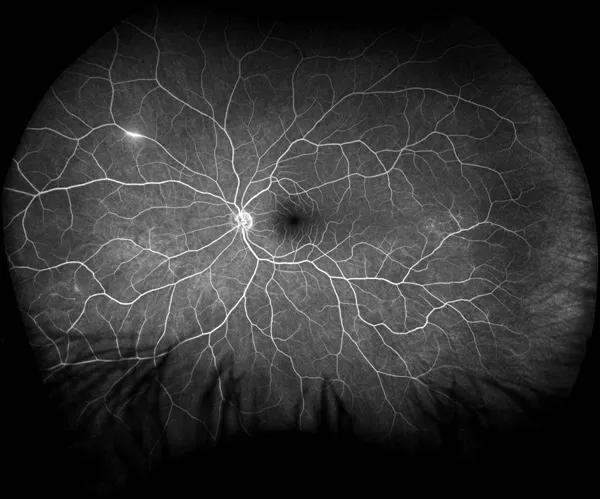
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/6f61581b-4387-4502-bd8b-c434ce7af7c8/17-EYE-1417-Sharma-CQD-Inset-2_jpg)
Figure 2. Ultra-widefield fluorescein angiogram of the left eye two months after presentation shows reperfusion of the BRAO, and a new area of vessel wall hyperfluorescence in the nasal periphery.
Susac syndrome, first described by John Susac, MD, in 1979, is an immune-mediated, occlusive microvascular endotheliopathy that affects the microvasculature of the brain, inner ear and retina, resulting in brain dysfunction (mainly headaches and cognitive dysfunction, but also a variety of other neurologic symptoms); hearing loss, tinnitus and vestibular dysfunction (vertigo); and visual disturbances, including scotoma, visual field deficits and BRAOs.
The typical and unique MRI finding is the presence of corpus callosum lesions, typically referred to as snowballs, best seen on T2 FLAIR images. In the retina, the occlusive disease most typically manifests as multiple BRAOs occurring over time, but can also be seen as segmental vessel wall hyperfluorescence/leakage, capillary dropout, peripheral nonperfusion and peripheral capillary changes.
Advertisement
In our experience, treatment for Susac syndrome needs to be prompt, aggressive and sustained. The mainstays of treatment include pulse IV methylprednisolone, followed by high-dose oral prednisone with tapering along with early introduction of IVIG and mycophenolate mofetil. The addition of IVIG and mycophenolate mofetil allows the oral prednisone to be tapered to prevent development of side effects associated with long-term prednisone therapy. In patients whose symptoms progress despite these treatments, it may be necessary to step up immunosuppression to include either rituximab or cyclophosphamide.
With aggressive treatment, symptoms can be controlled, preventing central nervous system decline and vision loss.
Dr. Sharma is a retina and uveitis specialist.
Advertisement
Advertisement

Motion-tracking Brillouin microscopy pinpoints corneal weakness in the anterior stroma

Registry data highlight visual gains in patients with legal blindness

Prescribing eye drops is complicated by unknown risk of fetotoxicity and lack of clinical evidence

A look at emerging technology shaping retina surgery

A primer on MIGS methods and devices

7 keys to success for comprehensive ophthalmologists

Study is first to show reduction in autoimmune disease with the common diabetes and obesity drugs

Treatment options range from tetracycline injections to fat repositioning and cheek lift