Advertisement
Analysis used echocardiographic data to assess structural valve deterioration
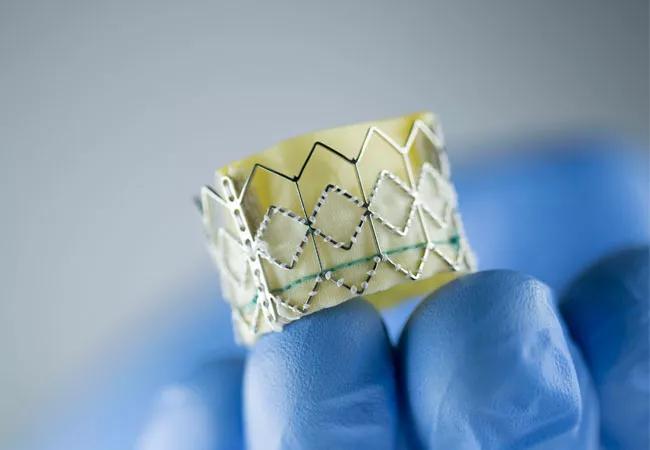
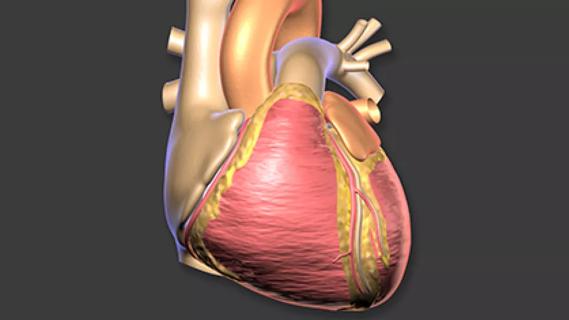
Transcatheter aortic valve replacement (TAVR) with the third-generation SAPIEN 3 balloon-expandable valve has demonstrated a five-year incidence of structural valve deterioration (SVD) similar to that with surgical aortic valve replacement (SAVR). So found an analysis of PARTNER 2 trial patients with severe aortic stenosis at intermediate surgical risk, recently published in the Journal of the American College of Cardiology (2020;76:1830-1843). The study found a higher rate of SVD in TAVR patients who received the second-generation SAPIEN XT balloon-expandable valve compared with SAVR patients.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“In this study, we used the new definition of structural valve deterioration using echocardiographic evidence, which is believed to more accurately reflect outcomes,” says study co-author Wael Jaber, MD, a Cleveland Clinic staff cardiologist. “Our findings have important implications for younger patients at intermediate surgical risk.”
TAVR is a well-established choice for symptomatic severe aortic stenosis in patients at high surgical risk. But for patients deemed to have intermediate or low surgical risk, results comparing TAVR with SAVR have been mixed: No significant difference was found in five-year incidence of death or disabling stroke in the PARTNER 2A trial, but in landmark analyses at two to five years after the procedure, a higher rate of death from any cause was found with TAVR. The third-generation TAVR valve (SAPIEN 3) has performed better than the second-generation valve (SAPIEN XT), which is no longer on the market.
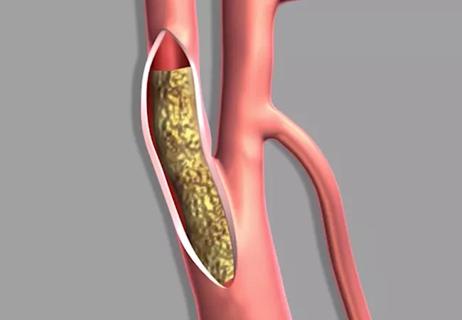
As more heart teams consider TAVR for lower-risk and younger patients with a longer life expectancy, valve durability is an issue of increasing concern. Historical definitions of SVD, based on valve reintervention or valve-related death, are thought to underestimate the incidence of valve deterioration by capturing only the most severe cases of SVD associated with symptoms. The more recent Valve Academic Research Consortium 3 (VARC-3) definition of SVD is based on identifying structural and hemodynamic valve deterioration using echocardiography. It is believed to better estimate the actual incidence of SVD and allow more accurate comparisons of aortic valve replacement options.
Patients who had echocardiographic data available were analyzed from the following two prospective multicenter studies:
The study population consisted of 891 patients who received the SAPIEN 3 valve, 774 patients who received the SAPIEN XT valve and 664 patients who underwent SAVR. All had symptomatic severe aortic stenosis and were deemed to be at intermediate surgical risk.
The primary endpoint was the incidence of SVD, using a modified VARC-3 definition: the composite of hemodynamic valve deterioration (stage ≥ 2) during echocardiographic follow-up and/or bioprosthetic valve failure related to SVD at five years.
Kaplan-Meier analysis found the following five-year rates of SVD:
Advertisement
At five years, rates of bioprosthetic valve failure were as follows:
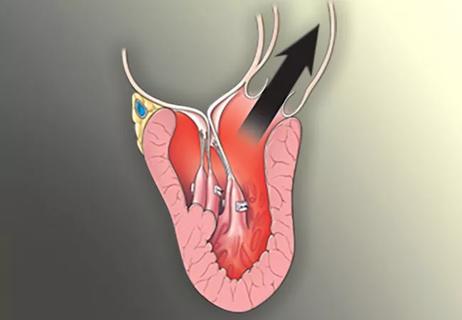
The main causes of bioprosthetic valve failure and valve reinterventions differed between cohorts. For patients who received SAPIEN XT, most were related to SVD. In contrast, for those who received SAPIEN 3, most failures and reinterventions were related to nonstructural dysfunction (i.e., paravalvular aortic regurgitation). Half of failures and reinterventions in surgical patients were attributed to endocarditis, with no endocarditis found in TAVR patients.
The 30-day mortality related to reintervention was significantly higher among surgical patients (50%) than in the TAVR groups (5% with SAPIEN XT, 0% with SAPIEN 3).
Advertisement
“Reinterventions for SAPIEN 3 failure were usually managed by transcatheter valve-in-valve procedures, whereas reinterventions in surgical patients predominantly required redo surgery, which drove up reintervention-related mortality in that group,” notes study co-author Samir Kapadia, MD, Chair of Cardiovascular Medicine at Cleveland Clinic.
The study’s multicenter team of authors concluded that evidence does not currently support choosing TAVR for all young, low-risk patients with severe aortic stenosis. But because five-year outcomes with the SAPIEN 3 valve were similar to those with SAVR, they deem TAVR with SAPIEN 3 to be a reasonable option in this patient group.
“These results increase our confidence in the durability of TAVR in patients at intermediate risk, at least through five years,” says Dr. Kapadia. “As time goes by, we’ll be able to evaluate longer-term outcomes.”
“Deterioration of the bioprosthesis after TAVR has been a concern from the beginning, so this analysis of early (up to five years) valve deterioration is important,” says Eugene Blackstone, MD, Head of Clinical Investigations in Cleveland Clinic’s Heart, Vascular & Thoracic Institute, who was not involved in the analysis. “Ten-, 15- and 20-year observations are of even more importance.”
Dr. Blackstone notes that he and others in the Valve Academic Research Consortium pointed out pitfalls of combining longitudinal hemodynamic data with time-to-event data in defining a composite time-related event for valve deterioration (JAMA Cardiol. 2017;2:1197-1206). “Longitudinal echocardiographic measurements of hemodynamics are inherently variable, depending on the patient’s condition, their heart function and inherent ‘noise,’” he says. “Trends of gradients or regurgitation over time are meaningful, but assigning a date to a specific threshold is fraught with uncertainty.”
He adds that bioprosthesis deterioration accelerates over time. “It therefore seems inappropriate to provide a series of estimates of a constant hazard and attach a P value to each year, as the current study does, rather than properly modeling the accelerating rate,” he says.
Advertisement
Moreover, Dr. Blackstone adds, patients in PARTNER 2 were elderly, and elderly people often die before their bioprosthesis has a chance to noticeably deteriorate. “This competing risk of death was not properly accounted for in this analysis,” he says.
Finally, Dr. Blackstone notes, whereas the current study presents data specific to two different SAPIEN prostheses, it presents SAVR data as if SAVR patients were a single homogeneous group. “In fact,” he observes, “the SAVR group included a heterogeneous variety of bioprostheses with a few mechanical prostheses thrown in. The valves include two with suspected or demonstrated early modes of failure — the Trifecta bioprosthesis (see Ann Thorac Surg. Epub 1 Oct 2020) and the MitroFlow bioprosthesis (see Eur Heart J Cardiovasc Imaging. Epub 13 Jan 2020). A consternation of the PARTNER trials has been that, unlike TAVR, which is largely an isolated procedure, the SAVR arms often included other components (e.g., coronary artery bypass grafting, mitral valve repair) and, with PARTNER 2, the surgeon’s choice of prosthesis.” Those choices, he says, could make a difference in average outcomes, such as the rate of bioprosthesis deterioration.
“All these concerns are ‘fixable’ and should be considered as we await the uncertain 10-year results with this new technology,” Dr. Blackstone concludes.
Advertisement
Advertisement

Surprise findings argue for caution about testosterone use in men at risk for fracture

Findings support emphasis on markers of frailty related to, but not dependent on, age
![GettyImages-1252287413 [Converted]](https://assets.clevelandclinic.org/transform/StoryPanel/350804b2-f1e4-4d97-a277-9629cf45af3e/23-HVI-4120348_redlining_650x450_jpg?w=3840&q=75)
Large database study reveals lingering health consequences of decades-old discrimination
Additional analyses of the two trials presented at 2023 ESC Congress
Prospective SPIRIT-HCM trial demonstrates broad gains over 12-month follow-up

An ACC committee issues recommendations to accelerate sluggish progress
Review of our recent experience shows it’s still a safe option
Machine learning may improve risk prediction and guide therapy