Case study: With a constellation of findings, OCTA proves best option in diagnosis
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 65-year-old woman presented for a second opinion to the Cole Eye Institute Vitreoretinal Service. She had been diagnosed with exudative age-related macular degeneration (AMD) and received four monthly bevacizumab injections, the most recent a month prior at an outside facility.
Her vision had not changed with any of the injections, and she was concerned about the course of treatment. On examination, she had minimal cataracts, and her visual acuity was 20/40 OD and 20/30 OS. Fundus photos revealed a greyish-white lesion OS and relatively normal examination OD without any drusen (Figure 1). The fluorescein angiogram (FA) showed early blocking with late leakage OS (Figure 2). Optical coherence tomography (OCT) showed minimal intraretinal changes and a characteristic subretinal lesion (Figure 3).
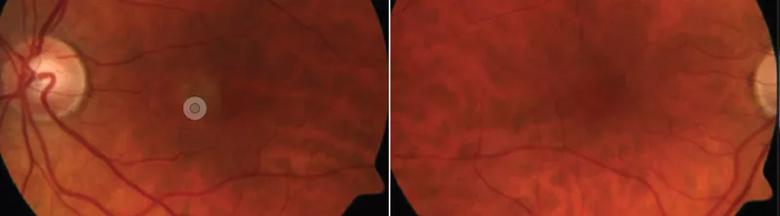
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/948ff6fc-4420-4883-8dcd-1eceafc6ff9e/17-EYE-1420-Kaiser-CQD-Inset-1_jpg)
Figure 1. Fundus photography shows a greyish-white lesion in the patient’s left eye, but her right eye appears normal. Notably, no drusen are seen.
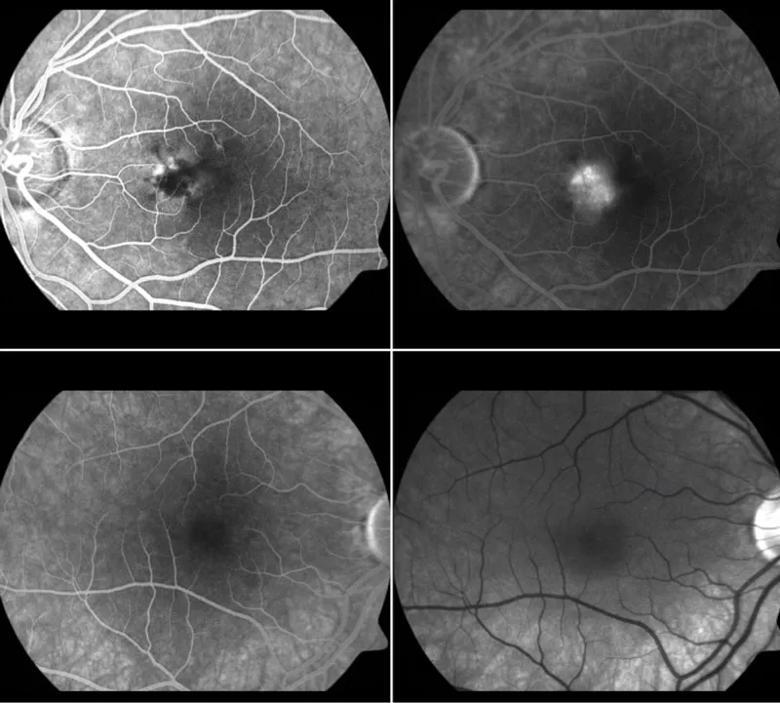
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/92e44966-9971-453d-9f35-802bba57ac4d/17-EYE-1420-Kaiser-CQD-Inset-2_jpg)
Figure 2. Fluorescein angiography shows early blockage with late leakage in the left eye. No staining of drusen is seen in the right eye.
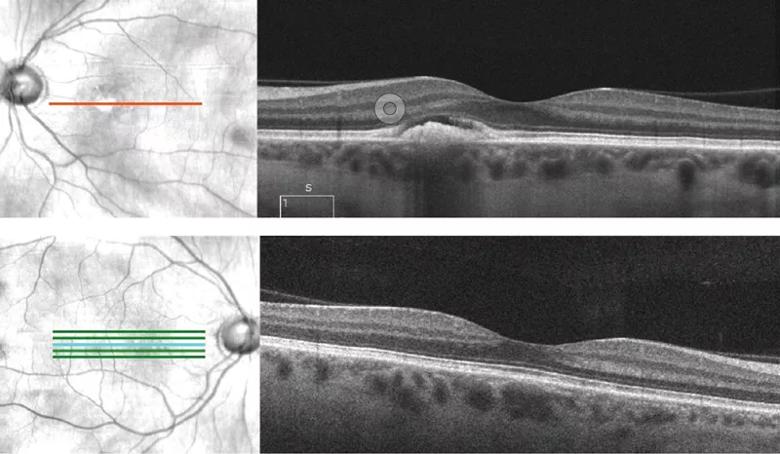
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ecd5408a-00e9-4f74-bbc9-1a0d01616137/17-EYE-1420-Kaiser-CQD-Inset-3_jpg)
Figure 3. Optical coherence tomography displays minimal intraretinal changes and a characteristic subretinal lesion in the left eye. The right is totally normal, with normal choroidal thickness seen in both eyes.
Is this examination enough to continue anti-vascular endothelial growth factor (VEGF) injections? Should we switch anti-VEGF agents? Should we add photodynamic therapy? The constellation of findings in this patient led to a differential diagnosis of wet AMD, pachychoroidal neovascularization, chronic central serous chorioretinopathy or adult-onset foveomacular vitelliform dystrophy. OCT angiography (OCTA) is the best option to differentiate these entities.First, the choroid was not thickened, making central serous chorioretinopathy or pachychoroidal neovascularization unlikely. However, it was not thinned as in most wet AMD eyes. OCTA (Figure 4) showed something that was suspicious, but not definitive for a choroidal neovascularization (CNV). This area was devoid of flow in the flow map, making CNV unlikely. Thus, we obtained a fundus autofluorescence image (Figure 5), which revealed the characteristic hyperautofluorescence from the lipofuscin accumulation seen in adult-onset foveomacular vitelliform dystrophy.
Advertisement
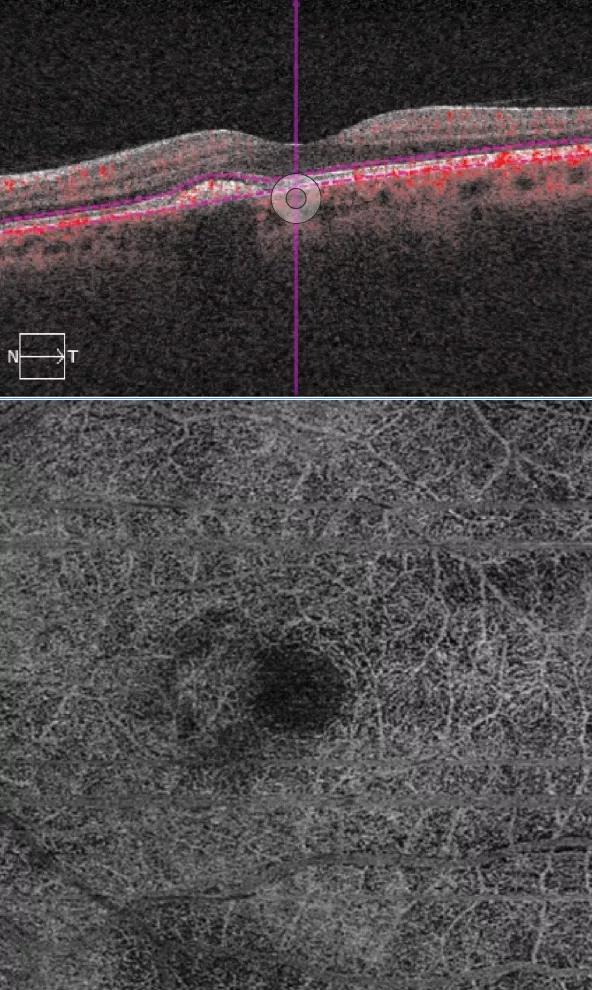
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/64d37dda-3c7c-4fb9-9448-639e0a528a35/17-EYE-1420-Kaiser-CQD-Inset-4_jpg)
Figure 4. Optical coherence tomography angiography reveals no flow within the lesion on the B-scan and no choroidal neovascularization in the en face image.
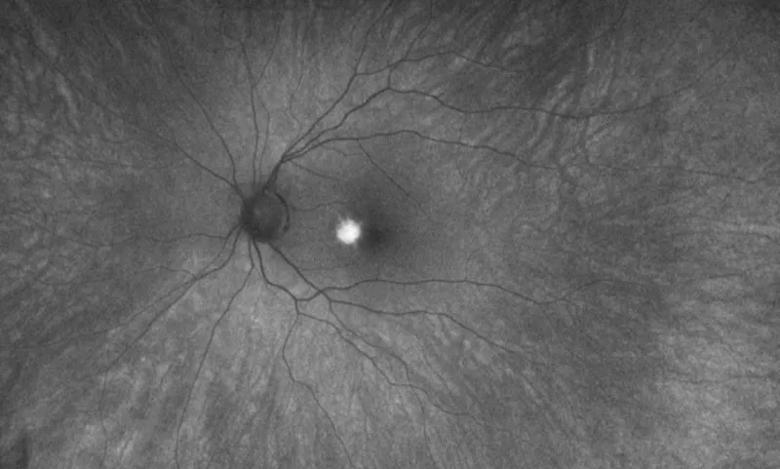
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/3ee05986-d781-4d83-a95f-fc368a64d3a9/17-EYE-1420-Kaiser-CQD-Inset-5_jpg)
Figure 5. Fundus autofluorescence reveals hyperautofluorescence from the lipofuscin accumulation typical of the vitelliform lesion in the left eye.Adult-onset foveomacular vitelliform dystrophy is the most common pattern dystrophy. It is characterized by subretinal yellow fluid that is above the retinal pigment epithelium on OCT. The FA in this case is very characteristic, and certainly the diagnosis could have been made based solely on the FA and OCT. CNV can be associated with pattern dystrophy, so it was very important in this case to rule it out. The prognosis is usually good, with rare loss of vision from CNV, geographic atrophy and macular holes.
We elected to stop the anti-VEGF injections given the lack of neovascularization. The patient has now gone for more than a year without any injections, progression of the lesion or change in vision.
Dr. Kaiser is a retina specialist and the Chaney Family Endowed Chair of Ophthalmic Research.
Advertisement
Advertisement

Motion-tracking Brillouin microscopy pinpoints corneal weakness in the anterior stroma

Registry data highlight visual gains in patients with legal blindness

Prescribing eye drops is complicated by unknown risk of fetotoxicity and lack of clinical evidence

A look at emerging technology shaping retina surgery

A primer on MIGS methods and devices

7 keys to success for comprehensive ophthalmologists

Study is first to show reduction in autoimmune disease with the common diabetes and obesity drugs

Treatment options range from tetracycline injections to fat repositioning and cheek lift