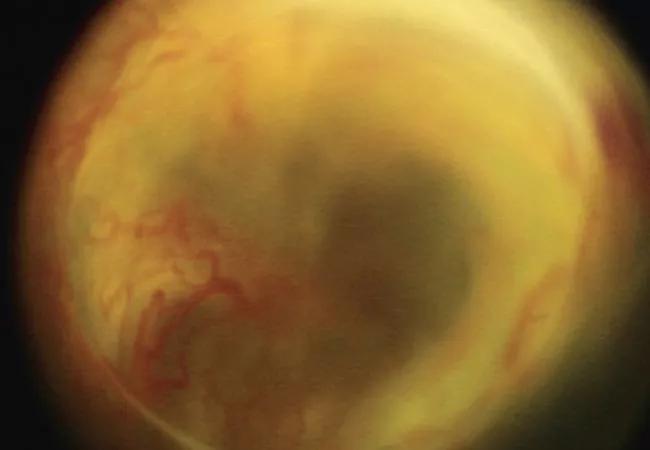
New study points to retinal metabolic remodeling and hepatic nitrogen imbalance
In retinopathy of prematurity (ROP) and other developmental eye diseases, science has shown two important truths:
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
That explains why the growth of endothelial cells, which form retinal blood vessels, is stunted in premature infants who require supplemental oxygen due to underdeveloped lungs.
But why these molecular changes occur hasn’t been well understood, specifically how hyperoxia changes cellular metabolism.
That’s what ophthalmic researchers at Cleveland Clinic have been working to reveal. For nearly two years they have studied the effect of hyperoxia in Müller cells, the only cells that produce the glutamine required for normal development of retinal endothelial cells and neurons.
Partial results were published recently in Nature Communications.
“We found that when we exposed Müller cells to high oxygen, not only was their capacity to produce glutamine decreased, but they started to consume glutamine themselves, depriving all other cell types in the retina,” says first author Charandeep Singh, PhD, a postdoctoral fellow at Cleveland Clinic. “This may be the primary mechanism of ROP.”
Dr. Singh and a team of researchers led by Cole Eye Institute ophthalmologist Jonathan Sears, MD, in collaboration with Henri Brunengraber, MD, PhD, of Case Western Reserve University, used mass spectrometry and stable isotope labeling to assess the molecular weight of biochemicals present in human and mouse Müller cells in both normoxic and hyperoxic conditions.
The team reported:
Advertisement
Studies in primary Müller cells from mice confirmed these findings, since immortalized cell lines like MIO-M1 are not always faithful in their function, noted Dr. Sears.
“Dr. Singh further definitively demonstrated that primary human brain cortical astrocytes, just like retinal Müller cells, used glutaminolytic carbon for the tricarboxylic acid cycle in high oxygen,” says Dr. Sears. “Moreover, he had a clever idea to demonstrate that hyperoxic retinal explants did not utilize acetate, something that central nervous system glia including retinal Müller cells usually utilize at a high rate to make citrate. This was surprising because it suggests that hyperoxia induces a widespread change to glutamine consumption in cells that normally synthesize glutamine for the basic metabolism and health of endothelial cells and neurons. It shows us that the eye reflects systemic disease.”
When Müller cells function under normal conditions, converting glutamate to glutamine, they also remove the toxic ammonium — a growth inhibitor — that other retina cells produce. However, in hyperoxia, when this process is reversed, Müller cells consume glutamine and actually produce more ammonium as a byproduct — twofold more.
So, what happens to the pathways, such as the liver-specific urea cycle, that can clear this ammonium from tissues? To find out, researchers studied the expression of two genes that encode rate-limiting enzymes of the urea cycle, Cps1 and Arg1, in primary hepatocytes from mice. They found that in hyperoxic conditions, these genes are downregulated, reducing hepatocytes’ capacity to quench ammonium.
Advertisement
“This hints that there also might be a malfunction in nitrogen metabolism in the liver during hyperoxia, which can exacerbate the phenotype we’re seeing in the retina,” says Dr. Singh. “Basically, high oxygen impairs the control of nitrogen systemically. This misregulation may contribute to a host of diseases, not just in the eye, but in the heart, lungs and more. In short, hyperoxia creates a nitrogen mess.”
More investigation is needed to confirm this liver-specific nitrogen imbalance before exploring pharmacologic means to address it by blocking or upregulating certain metabolic pathways.
In the retina, however, we now know that hyperoxia stimulates glutamine-fueled anaplerosis in Müller cells. This deprives retinal endothelial cells of glutamine, which is vital to their growth and function.
“Better understanding the effects of high oxygen on a cellular level, and how it stalls normal blood vessel development, will eventually help us better understand ROP, the leading cause of blindness in infants,” says Dr. Sears. “Preventing retinovascular growth attenuation and vaso-obliteration in response to hyperoxia of phase 1 of the disease ultimately will prevent ischemia or lack of blood flow of phase 2, thereby preventing pathologic, ischemia-driven neovascularization that leads to retinal detachment and blindness.”
Advertisement
Advertisement

Motion-tracking Brillouin microscopy pinpoints corneal weakness in the anterior stroma

Registry data highlight visual gains in patients with legal blindness

Prescribing eye drops is complicated by unknown risk of fetotoxicity and lack of clinical evidence

A look at emerging technology shaping retina surgery

A primer on MIGS methods and devices

7 keys to success for comprehensive ophthalmologists

Study is first to show reduction in autoimmune disease with the common diabetes and obesity drugs

Treatment options range from tetracycline injections to fat repositioning and cheek lift