JACC review calls for CMS to update coverage decision

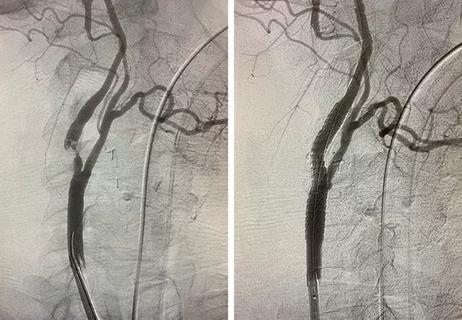
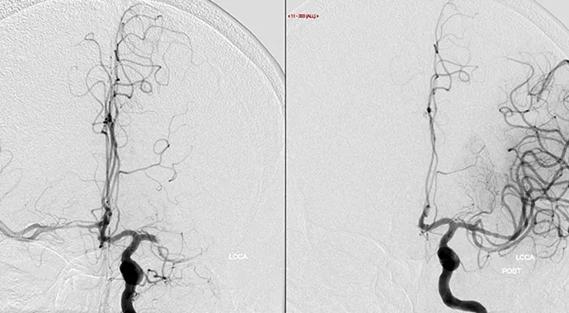
Outcomes of carotid artery stenting for stroke prevention in patients with carotid artery stenosis have reached parity with those of carotid artery surgery. So asserts a new JACC State-of-the-Art Review (J Am Coll Cardiol. 2022;80[2]:155-170), which attributes the parity to new techniques and devices, recent professional society statements promoting competency and improved understanding of appropriate candidate selection.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The review — written by a multicenter, multidisciplinary team of experts from across the U.S. after a comprehensive review of the literature — calls for the Centers for Medicare & Medicaid Services (CMS) to provide equal coverage for stenting and surgery for stroke prevention in patients with carotid artery stenosis.
“Few medical procedures have undergone as much scrutiny as carotid artery stenting,” says review co-author Sean Lyden, MD, Chair of Vascular Surgery at Cleveland Clinic. “Multiple randomized clinical trials involving more than 10,000 patients indicate that stroke and death rates associated with carotid artery stenting have decreased to levels similar to those with carotid endarterectomy.”
Introduced as an alternative to carotid endarterectomy in the mid-1990s, carotid artery stenting has demonstrated steadily improved outcomes since the last relevant CMS coverage decision was made in 2008. At that time, carotid artery stenting was regarded only as an alternative to patients deemed high risk for adverse perioperative outcomes with surgical intervention.
The reviewers conclude that carotid artery stenting has now demonstrated equivalence or noninferiority to surgery in periprocedural outcomes, long-term stroke prevention and durability. They attribute carotid artery stenting improvements to advances in the following areas:
Advertisement
“The evidence is now clear that carotid artery stenting is a reasonable and less invasive option than carotid endarterectomy for stroke prevention in patients with carotid artery stenosis,” Dr. Lyden notes. “However, it’s important that optimal strategies be employed, including the use of embolic protection devices, balloon sizing, efforts to ensure qualified operators, and appropriate candidate selection.”
The review also provides recommended treatment algorithms for carotid artery disease, including stenosis thresholds for carotid artery stenting. Thresholds are consistent with those of current FDA device approvals for patients with atherosclerotic bifurcation carotid disease at high and standard surgical risk, as follows:
Multidisciplinary team input can be invaluable when assessing risk, the authors note. A table in the article provides a list of clinical and anatomic features that confer elevated risk for either stenting or surgery. Overall, the lowest-risk option should be chosen, and in cases for which risk is deemed equivalent, the patient should choose.
“We advise educating patients to understand the options — including the role of optimal medical therapy — so they can knowledgeably weigh in on their preference,” Dr. Lyden observes.
Although about three-quarters of carotid artery revascularization procedures for primary stroke prevention are performed in asymptomatic patients, the benefit is not as well established in this group as in symptomatic patients. More evidence will be forthcoming from two large ongoing trials investigating outcomes for primary prevention in asymptomatic patients:
Advertisement
The reviewers also emphasize that carotid artery stenting is still evolving — more so than carotid endarterectomy, which has been an established procedure for many years. Continued developments in carotid artery stenting device technology, as well as in appropriate candidate selection and establishment of operator and institutional standards, can be expected to further lower risk.
In the meantime, Dr. Lyden and his colleagues recommend that CMS update its coverage decision to reflect that carotid artery stenting is as safe and effective as surgery. “CMS should not be putting Medicare patients at a disadvantage by favoring more invasive interventions, as it does with its current policy,” he says. “It’s time to bring coverage of carotid artery revascularization procedures in line with the evidence.”
“This excellent JACC State-of-the-Art Review summarizes the progression of carotid artery stenting from open-cell self-expanding to dual-layered stents, covering single and double embolic protection device use, vascular access, optimal patient selection, institutional criteria for operators, optimization of guideline-derived treatment and quality control for outcomes,” notes Cleveland Clinic interventional cardiologist Aravinda Nanjundappa, MBBS, who was not involved with the review. “It highlights the importance of multidisciplinary input and patient counseling while making decisions on carotid endarterectomy versus carotid artery stenting. The evidence shows an equipoise in clinical outcomes of the two approaches.”
Advertisement
Dr. Nanjundappa concludes: “In selected patients at high or average surgical risk for carotid endarterectomy, carotid artery stenting by experienced operators is a reasonable alternative to treat symptomatic and asymptomatic patients with carotid artery stenosis, consistent with FDA-approved stenosis thresholds. The CMS national coverage decision needs to be updated accordingly.”
Advertisement
Advertisement
A look at where TCAR and transfemoral carotid stenting are likely headed

Aim is for use with clinician oversight to make screening safer and more efficient

Tasked-based therapy improves social connection and quality of life

LAA closure may be compelling option in atrial fibrillation ablation patients at high risk of both stroke and bleeding

Case illustrates essentials of the low-risk, high-potential procedure when paired with rehab

New analyses confirm preservation of ablation outcomes, broaden data on bleeding benefits

Increasing treatment options are extending the window for continued functional gains
Study links large artery atherosclerosis and delayed presentation to poorer treatment results