New insights into old problems may change long-term outcomes

By Tara Karamlou, MD, MSc, and Hani Najm, MD, MSc
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Arch obstruction following the Norwood operation is an important problem that increases the risk of adverse short- and long-term outcomes.1,2 In fact, despite the relatively long surgical experience, recoarctation in neonates following arch repairs is a persistent and unsolved problem.
Measuring the true impact and prevalence of arch obstruction is challenging for a number of reasons, including:
First described by Norwood and colleagues in 1981, the Norwood operation is the first in a series of three operations that are used as standard therapy for neonates with hypoplastic left heart syndrome.3 One of the major components of this procedure is reconstruction of the hypoplastic arch with amalgamation to the pulmonary artery. Despite multiple iterative described techniques to reduce the prevalence of recoarctation following Norwood, the reported prevalence was still 17% in the NHLBI-Pediatric Heart Network-sponsored Single Ventricle Reconstruction (SVR) trial.4 Single-institutional studies have reported both much lower (0%) and much higher (46%) rates depending on the institution and the morphology of the patient population. Treatment for arch obstruction in this group is usually percutaneous balloon angioplasty; however, the efficacy of this procedure is variable. More importantly, the timing of deployment may critically influence the degree of physiologic recovery of the univentricular circulation – and therefore the eventual candidacy for Fontan completion.
Advertisement
Because of the important implications of this anatomic problem and the perception that such an issue is potentially modifiable, we investigated the determinants and time-related outcomes of arch obstruction in a prospective multi-institutional cohort of 593 neonates from 27 participating institutions, all of whom underwent the Norwood operation between 2005 and 2017 as part of the critical Left Ventricular Outflow Tract Obstruction study conducted by the Congenital Heart Surgeons’ Society (CHSS). Because many of these patients undergo repeated interventions to address coarctation, we used complex statistical models including modulated renewal analysis and multi-phase parametric modeling to elucidate the relationships between candidate risk factors and endpoints over time.
Concordant with the SVR trial, recoarctation was common in the early phase following Norwood (with a peak hazard at three months), with 146 neonates (26%) undergoing either catheter-based intervention or surgical reintervention. Unfortunately, 49 of these patients required a second intervention and 17 required a third reintervention. Although catheter-based therapy was most widely used, surgical intervention was more definitive at mitigating the risk of recoarctation.
Institutional practice was highly variable. The vast majority of surgeons used a medial incision on the undersurface of the arch with patch augmentation. Complete coarctectomy was used in 170 patients, with an end-to-side or end-to-end anastomosis concomitant with medial incision. The complete removal of ductal tissue is widely believed to be necessary to prevent later ductal constriction thought to be operational in recoarctation. A comparably new technique, interdigitation — used most commonly at two institutions — significantly decreased the risk of recoarctation (14%) compared with other distal arch reconstruction techniques (26%).5,6 This technique involves medial incisions in the ascending hypoplastic aorta, complete coarctectomy to remove all visible ductal tissue, and two longitudinal incisions in the anterior and posterior walls of the descending aorta. An extended end-to-end anastomosis is then performed, which increases the effective orifice of the distal neoaortic anastomosis and maximizes the contribution of native tissue.
Advertisement
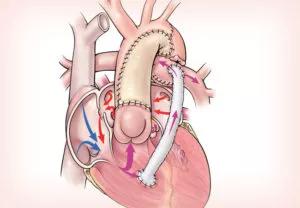
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/530ae2b5-0c55-430e-95e6-f090eef29606/19-CHP-994-NorwoodOperation-650x450-300x208_jpg)
Interestingly, we did not find an association between the shunt type (i.e., modified Blalock-Taussig shunt or right-ventricle-to-pulmonary-artery [RV-PA] conduit) to inform outcomes. We hypothesized that, owing to the relative fragility of the aortopulmonary shunt compared to the RV-PA conduit, the former group would have decreased physiologic tolerance for arch obstruction and higher mortality. This relationship and rationale has been intimated in an ad hoc analysis of the SVR trial data.7
It is promising that a reproducible technique for arch reconstruction in the Norwood operation seems to decrease the prevalence of recoarctation. This technique can be extrapolated to other forms of aortic hypoplasia, and will hopefully pay similar dividends to reduce recoarctation following neonatal repair, which is a problem that has confounded the congenital heart surgical community for decades. Although our study did not find an association with mortality, physiologic correlates such as systemic right ventricular dysfunction and increased grade of tricuspid valve regurgitation were associated with arch intervention, suggesting that the increased afterload will have deleterious long-term consequences on the durability of the univentricular circulation. Moreover, arch reintervention to relieve arch obstruction was common in this cohort, a proactive strategy that also may mitigate mortality risk.
The role of residual ductal tissue in mediating recoarctation risk continues to be debated and clarification of the importance of complete resection will help frame optimal surgical approaches. Fortunately, investigation of the mechanistic and biostructural underpinnings of the ductal phenotype is the subject of a proposed prospective study led by Cleveland Clinic in collaboration with the Suneel Apte, MBBS, DPhil, Lab at Cleveland Clinic Lerner Research Institute and the CHSS.
Advertisement
Surveillance and transparency in the reporting of Norwood outcomes beyond the early phase is paramount to understand the efficacy, safety and risks of implementing new therapies. These initiatives are being championed by multiple collaboratives in the congenital heart community, including the National Pediatric Cardiology Quality Improvement Collaborative (NPC-QIC) and Children’s Neurodevelopment Outcomes Collaborative (CNOC); Cleveland Clinic Children’s actively participates in both. Ultimately, it is only through such thoughtful and unified approaches that we will learn the potential wisdom of our [r]evolutionary steps.
Advertisement
Advertisement

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Multimodal evaluations reveal more anatomic details to inform treatment

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more