ACC/AHA panel also upgrades catheter ablation recommendations
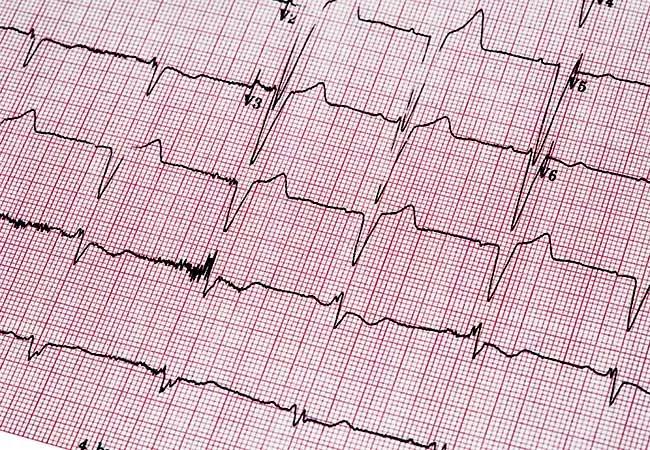
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b5f256a6-ea6c-4c72-8296-52cead849f08/23-HVI-4469361_atrial-fibrillation_650x450_jpg)
23-HVI-4469361_atrial-fibrillation_650x450
A new stage-based classification of atrial fibrillation (AF) and a greater emphasis on early rhythm control are among highlights of a new guideline on AF issued by the American College of Cardiology/American Heart Association (ACC/AHA) Joint Committee on Clinical Practice Guidelines.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The proposed classification is designed to better define AF as a progressive disease, breaking it into four stages:
In contrast, previous ACC/AHA guidelines from 2014 and their 2019 focused update defined AF in five terms: paroxysmal, persistent, long-standing persistent, permanent and nonvalvular.
“Our panel advocates viewing atrial fibrillation on a continuum, besides classifying and treating it based on arrhythmia duration or AF state, as was previously the case,” says Cleveland Clinic electrophysiologist Mina Chung, MD, who served as vice chair of the guideline writing committee.
The guideline also introduced anticoagulation decisions based on estimated stroke/thromboembolic risk, recognizing limitations in the traditionally used CHA2DS2-VASc score and allowing flexibility in the use of other scores and accounting for other stroke risk factors not included in CHA2DS2-VASc. “Many patients fall into the higher-risk categories, where it is clear that anticoagulation is recommended,” notes Dr. Chung, “but this guideline should be particularly helpful to clinicians faced with decision-making for individuals at lower risk who are in a gray zone when it comes to use of specific therapies such as anticoagulation.”
Advertisement
Additionally, in contrast to the 2014 guideline and 2019 update, the new guideline recommends a trial of rhythm control in patients with reduced left ventricular function and persistent AF to evaluate whether AF is contributing to left ventricular function. The guidance is similar to a rhythm control strategy favored in the latest European Society of Cardiology recommendations. “The field has been moving toward earlier rhythm control, and the current evidence and our recommendations reinforce the importance of that to reduce progression to persistent atrial fibrillation,” Dr. Chung explains.
An extensive literature review and an assessment of 11 previous ACC/AHA guidelines related to AF, with publication dates from 2014 to 2023, formed the evidence base for the recommendations, which were published in Circulationand the Journal of the American College of Cardiology. Writing group members included electrophysiologists, cardiologists, surgeons, pharmacists and patient representatives/lay stakeholders.
“At Cleveland Clinic, we’ve been on the cutting edge of atrial fibrillation treatment strategies and technology, particularly earlier rhythm control, and our investigators have participated in some of the studies that support the guidelines,” Dr. Chung notes.
AF prevalence in the United States is growing, with 12.1 million cases forecast by 2030. Among other adverse outcomes, the disease is associated with a 1.5-fold to twofold increased risk of death, which is somewhat higher in women than in men.
Advertisement
As noted by the panel, recent evidence consistently shows that optimal treatment of AF requires multiple stakeholders committed to providing comprehensive patient-centered care and a holistic view of the condition over an individual’s lifetime.
In addition to the new classification framework and the emphasis on early rhythm control, the ACC/AHA guideline authors identified several other take-home messages from their document:
Advertisement
The guideline also includes guidance for clinicians treating patients with AF who have renal failure, liver failure, heart failure, pregnancy or noncardiac illness. Anticoagulation receives a Class 1 recommendation for reduction of stroke risk in individuals at risk of stroke and stage III renal failure. Direct current cardioversion, the panel notes, is safe for pregnant patients. Counseling about the significant risk of recurrent AF is recommended for individuals in whom the condition is diagnosed during an acute medical illness or surgery.
“We want this guideline to be practical and prescriptive for clinicians,” Dr. Chung adds. “To that end, an app is being developed that focuses on take-home messages that represent a change in practice.” Already available online are a Guidelines-at-a-Glance article in the Journal of the American College of Cardiology (2024;83:280-284) and an interactive tool for catheter ablation as first-line therapy for rhythm control.
“This guideline update is a welcome addition to existing recommendations on how to manage this complex disease,” says Oussama Wazni, MD, MBA, Section Head of Cardiac Electrophysiology and Pacing at Cleveland Clinic. “It should be applauded for its attention to prevention and risk factor modification in addition to guidance on how to optimize therapy in all types of treatment strategies. Additionally, its strengthened endorsements for catheter ablation as first-line therapy in patients with paroxysmal atrial fibrillation and the use of left atrial appendage occlusion devices are good news for expanded use of these interventions for appropriate patients.”
Advertisement
Advertisement
LAA closure may be compelling option in atrial fibrillation ablation patients at high risk of both stroke and bleeding
UK experts compare and contrast the latest recommendations
While results were negative for metformin, lifestyle counseling showed surprising promise
Investigational pulsed-field ablation system also yielded procedural efficiencies
Concomitant AF ablation and LAA occlusion strongly endorsed during elective heart surgery
For the first time, risk is shown after accounting for underlying contributions of pulmonary disease
Retrospective analysis finds “hypoxic and sleepy” subtype to confer greatest risk
Network proximity and EHR analyses identify diabetes drug as a top candidate for risk reduction