Mounting support for the newly described microstructure from a 7T MRI and electroclinicopathologic study
The black line sign — a novel MRI marker for focal cortical dysplasia (FCD) type IIB — shows promise as a useful tool for planning intracranial EEG evaluation and surgery in patients with medically intractable FCD IIB. So concludes a Cleveland Clinic retrospective study of 20 patients with FDC II who underwent 7T MRI.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“We found that among patients undergoing resection for intractable focal epilepsy who had a 7T MRI with sufficient image quality, the presence of the black line sign suggested a high likelihood of FCD IIB,” says Irene Wang, PhD, corresponding author of the study, published in Neurology. “Moreover, the black line region was highly concordant with the intracranial EEG-defined seizure onset zone and was significantly associated with seizure freedom when it was included in resection.”
The black line sign, first reported in 2016 and named in 2019, is an intracortical hypointense band found in deep layers below apparently preserved upper cortical layers of the brain. “Although previously reported in 7T T2*-weighted images in patients with FCD IIB, detailed imaging and electroclinicopathologic characterization of this microstructure had been lacking,” says Dr. Wang, Research Director of Cleveland Clinic’s Epilepsy Center.
To provide such characterization, Dr. Wang and colleagues reviewed 7T T2*-weighted gradient echo images in a cohort of consecutive patients with pathology-confirmed FCD II intractable to medical therapy. They looked for occurrence of the black line sign and then assessed overlap between the black line region and the seizure onset zone as determined by intracranial EEG. They also determined whether inclusion of the entire black line region in the surgical resection was associated with seizure freedom after surgery. Additionally, they aligned histopathology specimens with the MRI to evaluate the black line sign’s pathological underpinnings.
Advertisement
“We also performed region-of-interest quantitative MRI analysis on 7T T1 maps in the black line region, the entire lesional gray matter, as well as the contralateral and ipsilateral normal gray matter and white matter,” Dr. Wang explains.
The black line sign was identified in 12 of 14 patients with FCD IIB (86%) and in none of six patients with FCD IIA (0%). Additional findings of note included the following:
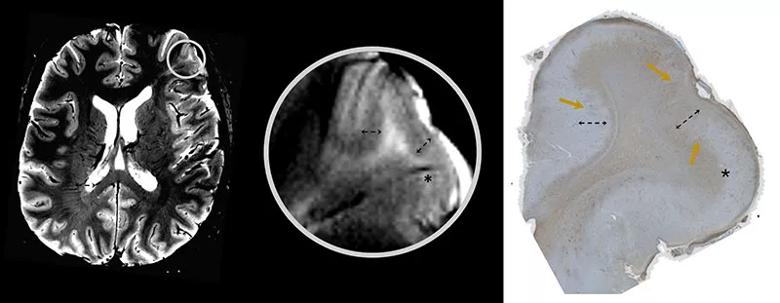
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/683f1569-7402-44a6-b7c4-d799b5072bac/22-NEU-3140066-CQD-Inset-800x311-1_jpg)
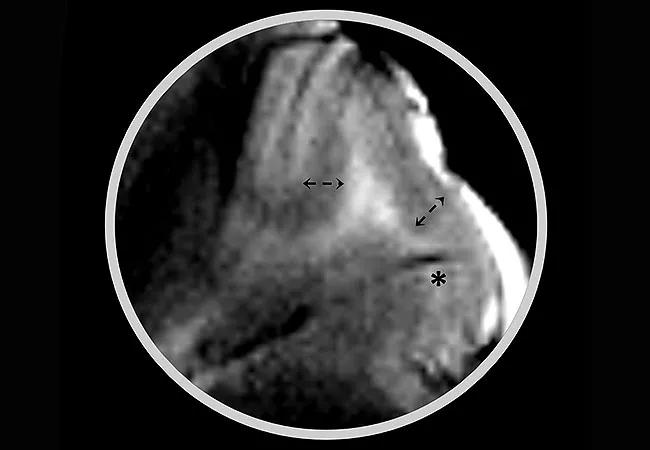
Figure. Illustration of the black line sign and its MRI-pathology correlation. Well-matched alignment between 7T T2*-weighted gradient echo images (left image: axial MRI with circle indicating the FCD IIB lesion; middle image: zoom-in of lesion showing the black line microstructure) and histopathology with vimentin stain (right image) showing balloon cells (yellow arrows) at the black line site (black dashed arrows). The star indicates vasculature nearby.
Dr. Wang notes that while the study is limited by its small size and retrospective nature, it yielded several compelling findings: (1) the black line sign was present in a large proportion of FCD IIB cases but absent in FCD IIA, (2) the black line region was highly concordant with the intracranial EEG-defined seizure onset zone and (3) full inclusion of the black line sign in resected tissue was strongly associated with seizure freedom.
Advertisement
“Taken together, these results suggest that the black line sign may ultimately serve as a neuroimaging marker for FCD IIB on ultra-high-field MRI,” Dr. Wang observes.
The authors point out that in the current study the black line sign’s subtyping performance surpassed that of the transmantle sign — the current best clinical marker of FCD IIB. They write: “Together, MRI features within the gray matter (such as the black line sign) and the white matter (such as the transmantle sign) could contribute complementary information to facilitate noninvasive FCD subtype prediction.”
The authors call for caution before crediting the seizure freedom in their study solely to removal of the black line region, since resection targeted removal of the whole lesion rather than just the black line region. They note, however, that at the very least their findings support consideration of the black line sign when planning the extent of resection — especially when removal of the entire lesion is not possible for practical reasons, such as proximity to eloquent cortex or vasculature.
Finally, Dr. Wang takes care to note that this study’s aim was characterizing microstructural features of FCD lesions, not whole-brain lesion detection. “We need to be cautious when using the black line sign for lesion detection in clinical settings, as false-positive rates have not yet been evaluated,” she says. “Sensitivity and specificity of this marker must be studied further in larger cohorts of FCD patients and controls.”
Advertisement
Advertisement

Novel Cleveland Clinic project is fueled by a $1 million NIH grant

Patients with epilepsy should be screened for sleep issues

Sustained remission of seizures and neurocognitive dysfunction subsequently maintained with cannabidiol monotherapy

Model relies on analysis of peri-ictal scalp EEG data, promising wide applicability

Investigational gene approaches offer hope for a therapeutically challenging condition
Study combines intracranial electrophysiology and SPECT to elucidate the role of hypoperfusion

Characterizing genetic architecture of clinical subtypes may accelerate targeted therapy

Data-driven methods may improve seizure localization and refine surgical decision-making