Cleveland Clinic team shares guidance, including use of backup mechanical support
Despite the risk of postcardiotomy shock, some patients with left ventricular failure due to ischemic cardiomyopathy can benefit from coronary artery bypass grafting (CABG) — with appropriate patient selection and precautions, such as anticipating possible need for mechanical circulatory support. So argues a team of four Cleveland Clinic cardiothoracic surgeons in a recent editorial in Innovations: Technology and Techniques in Cardiothoracic and Vascular Surgery (2021;16:227-230).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Most patients with ischemic cardiomyopathy are unlikely to return to normal left ventricular function after CABG, but an improvement in left ventricular ejection fraction, say from 20% to 35%, can have a significant impact on quality of life and life expectancy,” says lead author Michael Tong, MD, MBA.
He and his colleagues note that preoperative assessment of a patient’s suitability for CABG and anticipated improvement in myocardial function should address several key questions, outlined below.
If CABG is to do any good, the dysfunctional and ischemic myocardial territories should correspond to stenotic coronary segments. In general, target vessels should have stenosis greater than 70% with reasonable runoff and diameter large enough to pass a 5F angiography catheter.
Stunned or hibernating myocardium can possibly recover with revascularization, whereas scar tissue is irrevocably damaged. Myocardium without scar or with scar limited to no more than 50% of full wall thickness has the best potential to improve.
This is best assessed with magnetic resonance imaging (MRI) with delayed gadolinium enhancement (preferred) or, if this is not possible, with 18F-fluorodeoxyglucose positron emission tomography. “We prefer MRI because it can assess the thickness of myocardial scar, which in ischemic cardiomyopathy begins in a subendocardial pattern,” says editorial co-author Faisal Bakaeen, MD. He notes, however, that MRI can be difficult to obtain in patients who have renal dysfunction, are critically ill or have implanted devices.
Advertisement
Patients with a preoperative cardiac index greater than 2.2 L/min/m2 are likely to be able to come off of cardiopulmonary bypass without difficulty. In addition, a pulmonary artery pulsatility index greater than 1.8 indicates good right ventricular functional reserve. On the other hand, patients with poor right ventricular function — as reflected in a cardiac index less than 2.0 L/min/m2, pulmonary artery pulsatility index less than 1.2 or central venous pressure greater than 20 mmHg — should be assessed by a heart failure team and undergo hemodynamic optimization before CABG is attempted.
Patients with high transpulmonary gradients (> 15 mmHg) may need support with inhaled pulmonary vasodilators after CABG, or to forgo CABG. Further, if the pulmonary hypertension is secondary to left ventricular congestion, patients are more likely to have transpulmonary gradients less than 15 mmHg and high pulmonary capillary wedge pressure. These patients should have their medical condition optimized before surgery, and any valvular disease should be aggressively treated.
“These readings are typically available because we routinely do right heart catheterization in patients with severe ischemic cardiomyopathy,” Dr. Tong explains.
Being able to walk is a good sign. Patients with angina typically have viable myocardium, whereas those in whom shortness of breath predominates are likely to have lower cardiac indices and more advanced heart failure.
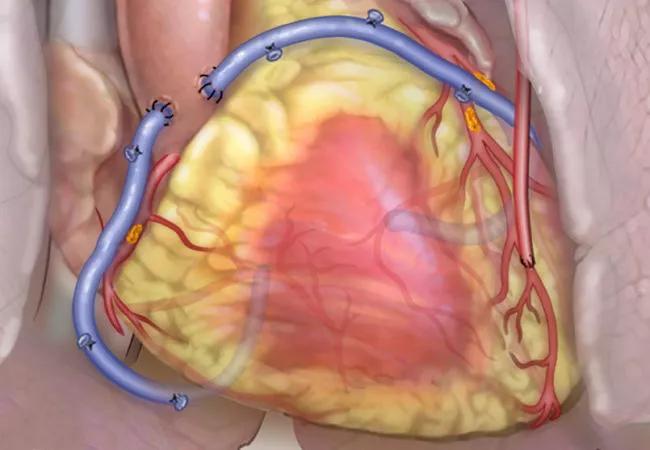
Not all patients with low ejection fraction will require temporary mechanical circulatory support, but a plan for such support should be in place. During CABG procedures in such patients at Cleveland Clinic, surgeons are prepared to insert a temporary mechanical support device, preferably the Impella 5.5, on a moment’s notice by preemptively opening the right axillary artery and sewing a 10-mm graft before initiating bypass. If an Impella is inserted, patients are weaned from the device afterward on an individualized basis; if they cannot be weaned, they are considered for placement of a durable left ventricular assist device (LVAD).
Advertisement
In fact, at Cleveland Clinic, patients with poor prognostic signs for postcardiotomy shock — such as a preoperative cardiac index less than 2.0 L/min/m2, poor right ventricular function and poor coronary targets — preoperatively undergo an abbreviated but formal advanced heart failure workup.
“In patients deemed to be at high risk of developing postcardiotomy shock, our heart failure team initiates an LVAD backup evaluation,” explains Jerry Estep, MD, Section Head of Heart Failure and Heart Transplantation, who works closely with the surgeons who wrote the editorial. “This consists of a physical exam, assessment of preoperative symptom burden and end-organ function, hemodynamic assessment and guideline-directed medical therapy, as well as screening for potential candidacy for durable LVAD or heart transplantation.” He adds that preoperative medical optimization is essential prior to high-risk surgery.
“We have found that preoperatively initiating evaluation for long-term circulatory support, including patient education, empowers patient and family decision-making and prepares them for this potential need,” adds editorial co-author Edward Soltesz, MD, MPH, Surgical Director of the Kaufman Center for Heart Failure Treatment and Recovery.
Patients return to the cardiothoracic surgery clinic six to eight weeks after surgery, and continue follow-up with an advanced heart failure team for the rest of their lives. Those with a residual ejection fraction lower than 30% or 35% are referred to the electrophysiology clinic. “This multidisciplinary team approach allows for complete assessment and longitudinal care,” notes co-author Aaron Weiss, MD.
Advertisement
Advertisement

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Multimodal evaluations reveal more anatomic details to inform treatment

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more