20 years of Cleveland Clinic experience in ~500 patients with proximal aortic aneurysm or dilation
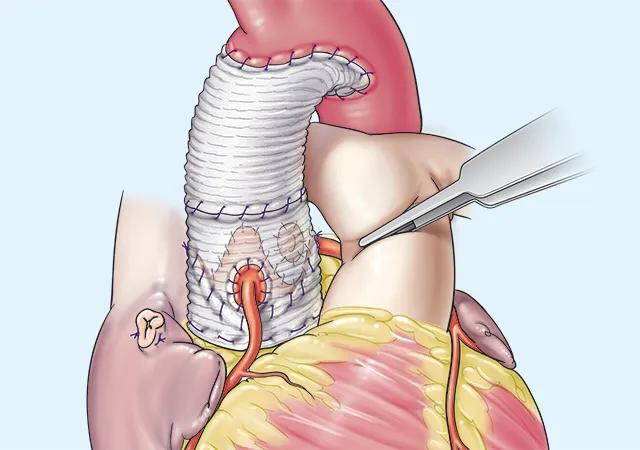
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/90aa9c96-4cde-4727-9afc-a9b394f127a1/19-HVI-1659827-Lars-Svensson-M-D)
completed aortic root replacement with reimplantation
For patients with a proximal aortic aneurysm or dilation, a modified aortic reimplantation technique —that is, reducing the anulus size to patient characteristics and creating neosinuses — results in excellent long-term survival and freedom from reintervention.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
So concludes an analysis of 20 years of data from 491 patients who underwent the operation at Cleveland Clinic. The series report, including a description of the surgical technique, was published online ahead of print in the Journal of Thoracic and Cardiovascular Surgery.
“The modified aortic reimplantation technique is reliable and reproducible,” says the article’s senior author, Lars Svensson, MD, PhD, Chief of Cleveland Clinic’s Heart, Vascular & Thoracic Institute, who is the surgeon who performed the operations in this series. “Because of the excellent long-term outcomes, I especially recommend this procedure for younger patients, who often have a connective tissue disorder.”
Patients with aortic root dilation have traditionally been treated with a composite valve conduit — i.e., aortic root replacement with a prosthetic aortic valve and graft. Also known as the Bentall procedure, it is associated with excellent long-term outcomes but carries risk of complications related to the prosthesis and bleeding if a mechanical valve is used. For patients with a viable aortic valve, Tirone David, MD, of the University of Toronto, who trained in cardiovascular and thoracic surgery at Cleveland Clinic, developed a technique to spare the valve.
More than 20 years ago, Dr. Svensson made changes to the valve-sparing operation with the goal of improving durability (Ann Thorac Surg. 2003;76[5]:1751-1753). The modified technique has the following critical features:
Advertisement
The newly published study was designed to evaluate late outcomes, i.e., after 15 years, among patients who underwent the procedure. Data from January 2002 to May 2023 were analyzed, during which 491 adults underwent the modified aortic reimplantation for aortic aneurysm or dilation at Cleveland Clinic by a single surgeon; operations on children and recent operations, totaling more than 528, were excluded.
Indications for surgery included any of the following:
Patients had a mean (± SD) age of 48 ± 14 years, and 82% were men. A connective tissue disorder was noted in 156 of 415 patients (38%), of which Marfan syndrome was the most common (n = 123). Among 478 patients, preoperative aortic regurgitation was characterized as mild in 22%, moderate in 29% and severe in 10%; the remaining patients had no aortic regurgitation. A small percentage of patients (4.3%; n = 21) had a bicuspid aortic valve.
No operative deaths occurred among the 491 patients in the study cohort, and the authors note that this 0% operative mortality continued through all 528 elective, modified aortic reimplantations conducted through January 2024. Among the 491-patient study cohort:
Advertisement
“These data show that long-term outcomes with modified reimplantation are excellent, with only 5% of patients requiring another operation within 15 years, mostly for an infection,” Dr. Svensson notes.
The article emphasizes the importance of anulus sizing for successful reimplantation, balancing the risk of too large an anulus (affecting long-term cusp apposition and the development of aortic regurgitation) and tying the left ventricular outflow tract sutures too tightly (possibly causing cusp erosion, stenosis or a fistula).
Each component of the aortic root is systematically evaluated intraoperatively to help direct the repair, using the mnemonic “CLASS” for commissures, leaflets, anulus, sinus and sinutubular junction.
“Our excellent long-term outcomes indicate that the modified aortic reimplantation operation should be considered especially for younger patients with enlarged aortic roots,” Dr. Svensson concludes. “Intervention should be done early, before a large root develops, which carries risks of cusp tears or more advanced aortic regurgitation. This operation is also an excellent option for patients with leaking aortic valves and three leaflets, even in selected patients without significant root enlargement.”
He adds that older patients and those with more severe aortic regurgitation likewise did well with the operation. Patients with a bicuspid aortic valve also did well, though he notes that this group with already compromised valves will require further analysis and long-term follow-up.
Advertisement
“These data illustrate the incredible evolution we are witnessing in valve-sparing root replacement surgeries,” adds study co-author Milind Desai, MD, MBA, Medical Director of Cleveland Clinic’s Aorta Center. “Because such ‘finesse’ operations are typically performed in younger patients who wish to preserve their native aortic valves for a multitude of reasons, a high degree of experience is required to ensure technical success and an excellent long-term survival. As a cardiologist, when I look into the eyes of a young patient and their family preoperatively, nothing is more important than to have confidence in a superb outcome from my cardiac surgery colleagues.”
Advertisement
Advertisement
Modified-Bentall single-patch Konno enlargement (BeSPoKE) optimizes hemodynamics, facilitates future TAVR
Experience-based takes on valve-sparing root replacement from two expert surgeons
30-year study of Cleveland Clinic experience shows clear improvement from year 2000 onward
Surgeons credit good outcomes to experience with complex cases and team approach
For many patients, repair is feasible, durable and preferred over replacement
In experienced hands, up to 95% of patients can be free of reoperation at 15 years
Experience and strength in both SAVR and TAVR make for the best patient options and outcomes
Ideal protocols feature frequent monitoring, high-quality imaging and a team approach