First-ever procedure restores patient’s health

In a first-of-its-kind procedure, a multidisciplinary Cleveland Clinic team has performed a triple-organ transplant to successfully treat a patient with alpha-1 antitrypsin deficiency (A1ATD).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
While the genetic disorder’s progression may necessitate lung and, less frequently, liver transplantation, this is the first known instance where renal complications in addition to pulmonary and hepatic end-stage disease led to simultaneous lung, liver and kidney replacement from the same donor for A1ATD.
Combined lung/liver/kidney transplants for other conditions have been performed only three times in the United States, according to records kept by the national Organ Procurement and Transplantation Network.
The procedure at Cleveland Clinic took place over two days in mid-February 2024, using organs from a single donor. The patient, a 64-year-old man, was discharged to home after a six-week hospital stay. His recovery since then has been uneventful and he continues to undergo rehabilitation and gain strength.
“Given the complexity and magnitude of the surgery, he has done extremely well,” said Kenneth McCurry, MD, Surgical Director of Lung and Heart/Lung Transplantation at Cleveland Clinic.
Transplanting lungs, liver and kidney all at once “requires multidisciplinary expertise,” Dr. McCurry said. “Very few centers in the United States do it. We're fortunate that we have very skilled programs that are adept at surgically and medically managing these cases. That allows us to offer [transplantation] to patients who are declined at other centers.”
Alpha-1 antitrypsin is a glycoprotein protease inhibitor (PI) manufactured in the liver and secreted into serum. Its normal function is to protect lung tissue by inhibiting the activity of neutrophil elastases released during inflammation, thus preventing proteolytic injury.
Advertisement
Mutations of the a1AT gene (SERPINA1) cause A1ATD. The majority of patients with the most clinically severe cases of A1ATD have genetic variations involving the Z allele.
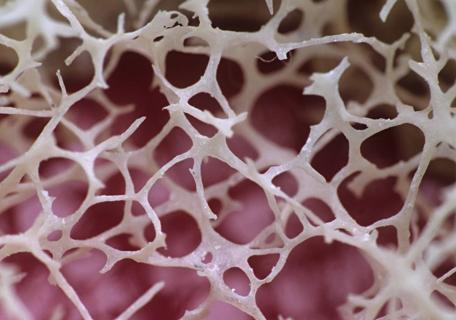
The mutant Z allele encodes malformed proteins that accumulate in the liver, causing tissue injury and scarring that can progress to cirrhosis. Insufficient production and secretion of properly configured A1AT also results in failure to inhibit proteolytic elastase in the lungs, leading to alveolar destruction and the onset of emphysema. Most A1ATD patients with liver disease are ZZ homozygous, a condition known as PIZZ. ZZ-homozygous patients also are at elevated risk for lung damage, especially if they smoke.
There are no medical treatments to reverse liver or lung damage in patients with A1ATD. Inhaled corticosteroids and bronchodilators, oxygen therapy and pulmonary rehabilitation make breathing easier, while augmentation therapy with IV infusion of donor-provided normal A1AT can prevent additional lung injury.
Patients with end-stage lung and/or liver disease can only be treated with transplantation. A successful liver transplant results in the normal production of A1AT, which eliminates future hepatic and pulmonary damage.
The patient with A1ATD who was referred to Cleveland Clinic in late 2023 for transplant evaluation had the PIZZ phenotype. He had smoked for 20 years before quitting in 2005. He developed emphysema and cirrhosis. At presentation, he had advanced liver, lung and kidney failure and had been undergoing dialysis for three months. His MELD (Model for End-Stage Liver Disease) score was 23.
Advertisement
His kidney dysfunction was primarily due to hepatorenal syndrome, a cascading condition and feedback loop in which cirrhosis and portal hypertension trigger waves of neurohormonal releases, systemic vasodilation, compensatory mechanisms, reduced cardiac output, renal vasoconstriction and renal hypoperfusion. The culmination is renal failure.
The patient experienced ascites and had undergone paracentesis on several occasions to evacuate fluid and relieve pressure in the abdomen.
“Given his history and end-stage kidney, lung and liver disease, his one-year prognosis was quite poor without transplantation,” Dr. McCurry said.
The decision to move forward with transplantation involved several considerations. They included the patient’s existing pulmonary hypertension and previous hemicolectomy; the potential negative impact of lung transplantation on postoperative kidney function; and the possibility of primary graft dysfunction in the transplanted lungs and/or liver.
“An important consideration is the patient’s motivation and their family and social support,” said Cleveland Clinic pulmonologist Sameep Sehgal, MD. “A triple-organ transplant is a massive endeavor. The recovery process can take months.”
Ultimately, the transplant teams determined that the patient was a viable multi-organ transplant candidate.
“We felt confident technically that we could successfully perform the procedures based on the skills of our various teams,” Dr. McCurry said, “and we felt comfortable that we could manage the patient’s care afterward.”
Advertisement
Cleveland Clinic registered the patient on the national transplant waiting list in two ways: as needing single-donor lungs, liver and kidney, and needing only single-donor lungs and liver.
“We preferred the first option,” Dr. McCurry said, “but we had decided that if lungs and liver were available without a kidney and we thought they were viable, we would proceed and then try to do a staged kidney transplant a few months later, after recovery.”
In the past, waiting periods for patients needing multi-organ transplants have been lengthy due to the scarcity of donors and organ allocation practices.
Recent changes to the national organ allocation system’s policies prioritized multi-organ transplant candidates and standardized and clarified when organ procurement organizations are required to allocate multiple organs to a single candidate.
“Historically, we were doing several heart-lung and lung-liver transplants per year at Cleveland Clinic, but those numbers were largely due to our ability to successfully utilize organs from donors that other transplant centers had declined,” Dr. McCurry said. “The recent policy changes will help facilitate additional multi-organ transplants. In our patient’s case, he was listed in December 2023 and was transplanted in mid-February,” when a matching single donor’s lungs, liver and kidney became available.
The lung and liver transplants were performed first, with the kidney transplant taking place several hours later, after confirmation that the patient was hemodynamically stable.
Advertisement
To begin, Dr. McCurry and the lung transplant team incised the patient’s chest and connected and initiated the venoarterial extracorporeal membrane oxygenation (ECMO) circuit. They removed the native left lung, then anastomosed, de-aired and reperfused the donor left lung, verifying hemostasis. The same procedure was followed for the right lung. Both donor lungs were ventilated and the patient was weaned from ECMO without difficulty, showing excellent lung function.
To ensure the donor lungs fit properly, Dr. McCurry slightly reduced their size using a stapler to perform wedge resections of the lingula and upper and middle lobes.
After chest closure, Koji Hashimoto, MD, PhD, Cleveland Clinic’s Director of Liver Transplantation, and his team began the liver transplant.
“To safely perform the liver transplant, we used machine perfusion to preserve the donor liver while the lung transplant was completed,” Dr. Hashimoto said. “Traditionally, donor organs are preserved in cold solution, where organ viability declines as ischemic time increases. With machine perfusion, the donor liver is perfused with warm oxygenated blood infused with nutrients. We can keep the organ viable and healthy until it is ready to be implanted. This machine perfusion technology is now our standard of care.”
After making a bilateral subcostal incision with a midline extension and entering the abdominal cavity, Dr. Hashimoto encountered adhesions from the patient’s prior hemicolectomy. These were carefully divided, then the surgeons proceeded with dissection to allow removal of the native liver and implantation of the donor liver using the piggyback technique.
They combined the recipient’s three hepatic veins to create a venous cuff for anastomosis with the donor liver’s suprahepatic vena cava. Anastomoses of the portal vein, hepatic artery and bile duct followed, interspersed with rounds of reperfusion of the graft and confirmation of hemostasis. After installing drains, the surgeons sutured the patient’s abdominal cavity and skin. He was transported to the cardiothoracic intensive care unit for monitoring.
Approximately eight hours later, the patient was returned to the operating room for kidney transplantation by Venkatesh Krishnamurthi, MD and his team.
After making the abdominal incision and during dissection and exposure of the abdominal cavity, the surgeons encountered an inguinal hernia. They repaired the defect, then continued with retraction and vascular clamping. The native kidney was excised. The donor kidney was implanted and anastomosed and the vascular clamps were released, resulting in prompt reperfusion and hemostasis. The surgeons trimmed the donor kidney’s ureter and anastomosed it to the patient’s bladder. They sutured a subcutaneous drain into place and closed the abdomen.
Managing the patient’s post-transplant immunosuppression routine required close collaboration among the three transplant teams.
“In general when we do combined lung and liver transplants, our lung transplant service manages the patient,” Dr. McCurry said. “The lungs are more immunogenic, with a higher rate of rejection episodes. As a result, we run immunosuppression levels a bit higher in this patient population.
“Because the kidneys are susceptible to injury from exposure to calcineurin inhibitors, particularly tacrolimus, our kidney transplant team manages immunosuppression somewhat differently,” he said. “With this patient, we used an interleukin-2 receptor antagonist for induction to allow us to reduce tacrolimus levels for a period of time so the donor kidney could recover.”
The patient spent several weeks in the intensive care unit following the surgeries.
“His lung and liver function were good,” Dr. McCurry said. “His kidney function lagged a bit but then improved and ultimately did fine. He required a tracheostomy, which we sometimes do to help patients wean from the ventilator. We usually wait about a week and if they're not extubated by that time, we move the breathing tube from the mouth to the trachea. It makes the patient more comfortable.”
The patient was discharged to home after six weeks.
“He was extremely motivated to get through this,” Dr. McCurry said. “He had worked hard to maintain his strength before the transplant, despite his declining status and weight loss. We learned a lot about his character and resilience.”
“Overall, the patient is doing very well at this time,” said Dr. Sehgal. “His lung function is over 100%, so it's better than normal. His liver and kidney function are also normal. He's been going through rehabilitation, getting stronger and trying to get back to a regular life as much as possible. He and his family have benefited from someone's generous decision to donate their organs after they've passed.”
The transplant’s successful outcome should be encouraging to other patients with similar conditions who previously may have been considered untreatable, Dr. Hashimoto said. “With careful patient evaluation and the expertise of our transplant team, we can make the untreatable treatable.”
Advertisement

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more

Insights on bringing Cleveland Clinic even closer to becoming the best transplant enterprise in the world

Consensus statement aims to increase use of the perfusion technology and raise transplant volumes

Minimally invasive pancreas-kidney replacement reduces patient’s pain, expedites recovery

AHA recommendations for pretransplant evaluation, peritransplant and long-term management

The agent-based model aims to improve prediction accuracy

New guidelines expand on psychosocial, sexual health, cognitive and other issues
Consensus conference begins work on new recommendations for clinical care and research