Multidisciplinary treatment of rare and complex immunodeficiencies
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 36-year-old female presented to Cleveland Clinic Respiratory Institute’s Immunology Clinic as a referral for immune dysfunction. Her medical history had been unremarkable except for a recent fall from her horse. Testing in an outside emergency department had uncovered a platelet count of 46 k/uL. She was then diagnosed with immune thrombocytopenia (ITP) and treated appropriately. She was referred to our clinic for long-term management.
Our clinic ordered further lab testing, which revealed an IgG of 191 mg/dL, an IgA of 26mg/dL and an IgM of 55 mg/dL. After showing poor response to multiple vaccine challenges, she was diagnosed with Common Variable Immunodeficiency (CVID) and began intravenous IgG.
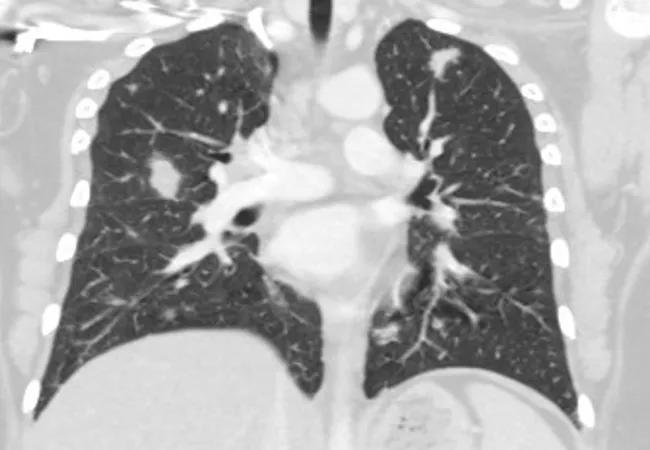
Soon after, she developed bloody diarrhea. Abdominal computed tomography (CT) showed multiple lung nodules and diffuse adenopathy. A CT chest confirmed the nodules.
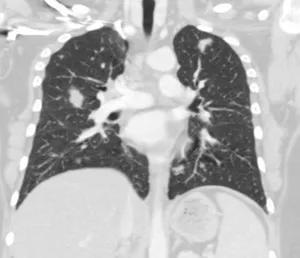
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5f6593bf-25e5-4554-baee-981b2ec1a3d8/Figure-1-a-fernandez-large-300x258_png)
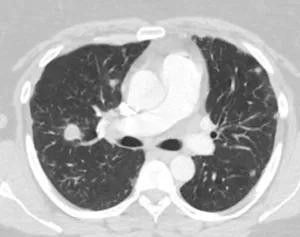
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/07328e53-7cb9-41d8-b086-db80bcc4db33/Figure-1b-fernandez-large-300x237_png)
Pre-treatment. CT chest shows numerous bilateral upper lung and lower lung pulmonary nodules without cavitation or calcification, measuring up to 17 mm.
Fecal analysis showed camphylobacter and Shiga toxin-producing E. coli, and an infectious disease specialist prescribed levofloxacin. Axillary lymph node biopsies showed follicular hyperplasia. Shortly after, she developed worsening shortness of breath. An open lung biopsy showed chronic lymphocytic bronchiolitis with areas of organizing pneumonia and lymphoid hyperplasia.
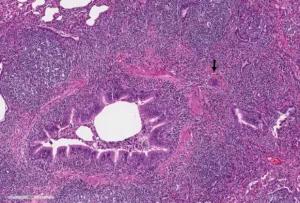
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b70916bc-66fb-4b2c-bd08-7a34f96f6b1f/figure-2-a-fernandez-large-300x203_png)
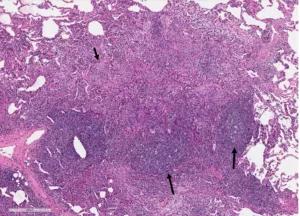
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/15a6b1ca-21ae-4951-9bd2-12f041bce8b2/Figure-2b-fernandez-large-300x216_png)
Wedge biopsies of upper and lower lobes of right lung. A. Lymphocytic bronchiolitis with a giant cell (arrow). B. Organizing pneumonia characterized by alveolar plugs of fibromyxoid tissue (short arrow) in association with the lymphoid follicles (long arrows).
Advertisement
Managing a patient with CVID, lung nodules and lymphadenopathy with potential for lymphoma requires a multidisciplinary approach. About one-third of patients with CVID have developed chronic pulmonary disease by the time of diagnosis. Furthermore, lymphomas also occur at much higher rates in patients with CVID, so a lymph node biopsy is important early in the course of treatment. A swift diagnostic and treatment approach is important in all immunodeficient patients.
This patient’s disease was originally treated with prednisone and had responded well, but shortness of breath recurred upon weaning to 5 mg every other day. Her reactive lymphadenopathy also responded well to the steroids.
The patient was presented at a weekly interstitial lung disease (ILD) clinic meeting, and the team decided to treat her with rituximab. Shortly thereafter, she received her first course, with excellent response clinically and radiographically. She receives periodic dosing (approximately once a year) of rituximab with continued control of her respiratory disease.
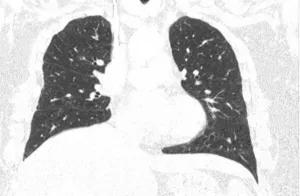
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/af9c3ee2-fc79-4616-a244-192aa956e0bc/figure-3a-fernandez-large-300x196_png)

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/3b8885d4-fdd1-4e3a-bb70-a3e5be7871ed/figure-3b-fernandez-large-300x265_png)
CT chest showing significant improvement in number and size of pulmonary nodules.
This patient is one of the many with rare and complex immunodeficiencies seen in our immunology and ILD clinics each week. This expertise has allowed Cleveland Clinic to build a team approach with immunologists, pulmonologists, hematologists, oncologists and other subspecialty physicians that are uniquely familiar with these types of patients.
Dr. Fernandez is staff in the Department of Allergy and Clinical Immunology.
Advertisement
Advertisement

Recent breakthroughs have brought attention to a previously overlooked condition

A review of treatment options for patients who may not qualify for surgery

Looking at the real-world impact and the future pipeline of targeted therapies

The progressive training program aims to help clinicians improve patient care

New breakthroughs are shaping the future of COPD management and offering hope for challenging cases

Exploring the impact of chronic cough from daily life to innovative medical solutions

How Cleveland Clinic transformed a single ultrasound machine into a cutting-edge, hospital-wide POCUS program

Collaborative patient care, advanced imaging techniques support safer immunotherapy management