Pulmonary endarterectomy improves outcomes for many patients
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 79-year-old man with chronic thromboembolic pulmonary hypertension (CTEPH) presented at Cleveland Clinic’s Respiratory Institute. He had been diagnosed previously with diabetes and atrial fibrillation. He had class III dyspnea, but the result of pulmonary function testing was normal. His 6-minute walk distance was moderately compromised. On echocardiography, his right ventricle appeared normal but with moderate tricuspid regurgitation. Estimated right ventricular systolic pressure was severely elevated, 71 mm Hg. Right heart catheterization showed a mean pulmonary arterial pressure of 40 mm Hg, wedge pressure of 15 mm Hg, cardiac output of 4.45 L/min and pulmonary vascular resistance of 5.6 Wood units despite pulmonary hypertension-targeted medical therapy. Careful review of the ventilation-perfusion (VQ) scan (Figure 1), computed tomography pulmonary angiography and conventional digital subtraction pulmonary angiogram (Figure 2) revealed bilateral surgically accessible disease.
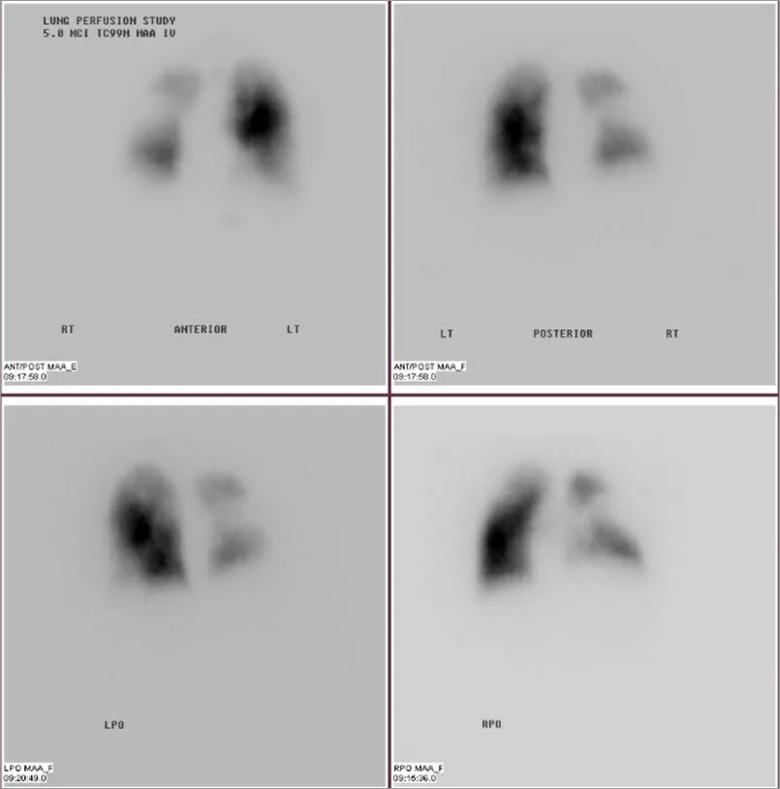
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ddb40460-125b-408c-9e67-96cce950d02d/805x-Inset-1-Chronic-thromboembolic-pulmonary-hypertension_jpg)
Figure 1
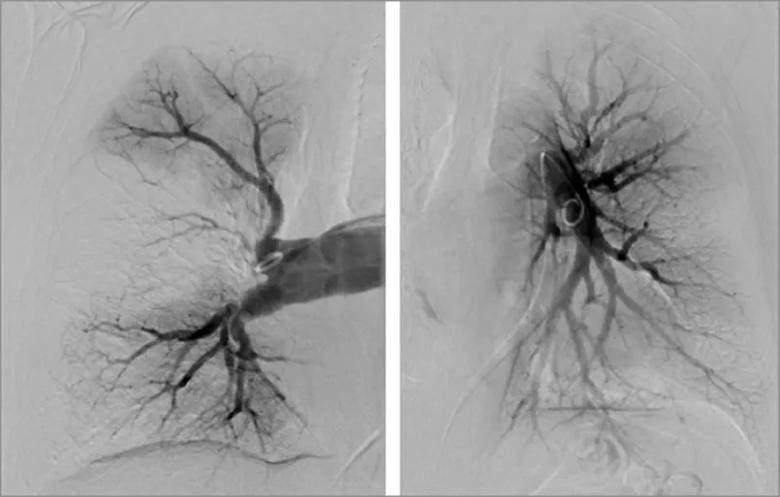
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d9ae2f39-6561-4eee-abe7-bcd143541060/805x-Inset-2-Chronic-thromboembolic-pulmonary-hypertension_jpg)
Figure 2
This patient was reluctant to pursue surgery, specifically pulmonary endarterectomy (PEA), and had been told that his risk was too high for balloon pulmonary angioplasty (BPA) because of his age and comorbidities.
During a virtual visit with this patient, we educated him on the benefits of PEA for someone with his condition. We reassured him that his comorbidities did not contraindicate the surgery and that PEA is a proven procedure with very low mortality when performed at an expert CTEPH center.
Advertisement
Nine months after PEA, the patient’s dyspnea had improved to class I-II. His mean pulmonary arterial pressure was reduced to 27 mm Hg, and he no longer needed medication to control pulmonary hypertension. The photo below shows the extracted specimen from the procedure.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/fe4c7a7d-b6e2-4985-9425-c15e855acf32/805x-Inset-3-Chronic-thromboembolic-pulmonary-hypertension_jpg)
Many patients have misconceptions about PEA, a complex surgical procedure that is often the preferred treatment for CTEPH. Patients should be referred to expert CTEPH centers for assessment and counsel on appropriate treatment.
At the 2020 CHEST® Annual Meeting, I discussed the value of seeking patient care at an expert CTEPH center. Expert centers offer:
While there are no official guidelines defining an expert center, there is consensus on expert center characteristics, which include advanced experience in:
An experienced multidisciplinary team, including surgeons, pulmonologists, radiologists, intensivists, perfusionists, respiratory therapists and interventionalists, is also characteristic.
Expert centers perform more than 50 PEAs annually and have surgical mortality under 5%. They also offer other treatment modalities, including BPA and medical therapy, since patient care sometimes requires a combination of treatments.
Accurate diagnosis is the first step in determining appropriate treatment. And often it requires the specialization of CTEPH experts.
Advertisement
The absence of a prior history of pulmonary embolism (PE) does not rule out CTEPH. The recommended screening test for CTEPH is the VQ scan. Segmental or larger perfusion defects that are not matched by ventilation defects may indicate CTEPH. On CT scan, CTEPH lesions may not appear as PEs but can be more subtle. Findings can be confirmed by pulmonary angiography and sometimes by MRI.
This combination of imaging helps determine the extent of disease. It also ensures that a CTEPH diagnosis is not confused with other conditions that can mimic it, such as:
According to a U.K. study of 550 patients with CTEPH treated from 2001 to 2014, those who had PEA had better 5-year survival than those who were able to have PEA but declined it. Data at Cleveland Clinic echo these results. From 2009 to 2019, 5-year survival of patients having PEA was 91.1% compared to 68.2% in nonoperated patients.
Not all patients are eligible for PEA due to the location of the lesion. That’s when BPA can be useful. But, unlike PEA, BPA typically requires multiple sessions. It’s also not without complications. Lesions in the microvasculature are best treated with medication. Some cases of CTEPH require a combination of treatments, a multimodality approach that is increasingly used by expert centers.
Patients who survive pulmonary embolism or deep vein thrombosis or patients with shortness of breath not explained by routine testing should be referred to an expert CTEPH center with multidisciplinary care including detailed diagnostics and all forms of CTEPH therapy.
Advertisement
Dr. Heresi is Director of the Pulmonary Vascular and Chronic Thromboembolic Pulmonary Hypertension Program within Cleveland Clinic’s Respiratory Institute.
Advertisement
Advertisement
Takeaways from the most recent annual meeting centered around clinical advances, AI integration and professional development
Recent breakthroughs have brought attention to a previously overlooked condition
A review of treatment options for patients who may not qualify for surgery
Looking at the real-world impact and the future pipeline of targeted therapies
The progressive training program aims to help clinicians improve patient care
New breakthroughs are shaping the future of COPD management and offering hope for challenging cases
Exploring the impact of chronic cough from daily life to innovative medical solutions
How Cleveland Clinic transformed a single ultrasound machine into a cutting-edge, hospital-wide POCUS program