A multidisciplinary approach to treatment can be beneficial since other organs in addition to the lungs can be affected by the systemic disease
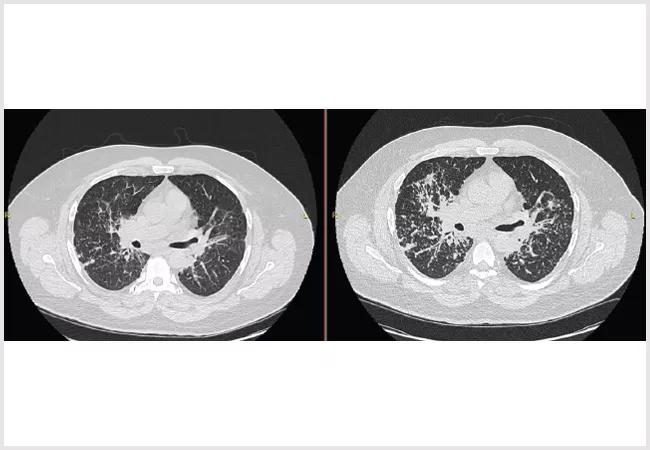
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e8939fe2-9330-42a9-8200-a96d22f0b871/22-PUL-3009526-CQD_Sarcoidosis-Case-Study-Lumpkin_jpg)
Sarcoidosis
Written by Timothy Lumpkin, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 54-year-old male originally presented after pre-operative testing for an upcoming orthopedic surgery. The test showed an abnormal CXR prompting further work up with CT chest and subsequent bronchoscopy. A lymph node biopsy demonstrated granulomas consistent with a diagnosis of sarcoidosis.
He was referred to the Cleveland Clinic for sarcoidosis. At the initial visit, he had normal spirometry without obstruction, forced vital capacity of 88% and DLCO of 102% and was asymptomatic. He was followed serially for a year until developing shortness of breath. Repeat imaging demonstrated progressive interstitial disease, and repeat pulmonary function testing showed new moderate obstruction and a drop in FVC to 79% predicted.
The patient was started on steroids and methotrexate. Steroids were weaned off after three months, and methotrexate was titrated to the appropriate dose over several months. After one year of therapy, his CT demonstrated significant improvement, and pulmonary function testing demonstrated resolution of his obstruction and a FVC of 95% predicted. In addition, his symptoms had resolved.
Sarcoidosis is a multisystem granulomatous disease of unknown etiology involving the deposition of non-necrotizing granulomas into involved organs. In nearly 90% of cases, the lungs are affected. Diagnosis involves an appropriate clinical picture, the exclusion of other etiologies and tissue sampling in some cases. Once diagnosed, clinicians must decide if and when to treat, which can be difficult given the systemic nature and varied presentation in each patient.
Advertisement
Treatment is aimed at preventing lasting disability from organ involvement and improving the patient’s quality of life. This involves targeting the immune system as it is inappropriately activated in this disease. Immunosuppressants such as steroids, methotrexate, leflunomide, azathioprine and TNF blockers have been used with success.
It’s important to consider that despite a predominance of cases involving the lungs, other organs can be involved as well. Nearly 30 % of patients present with extrapulmonary manifestations. The appropriate screening modalities for other organs involved have not yet been defined, but appreciating the complexity and spectrum of the disease is essential for holistic management. This is most easily achieved with a multidisciplinary approach, which is used at the Cleveland Clinic. Close follow-up with physicians familiar with the disease is essential in monitoring the disease and determining treatment options.
Advertisement
Advertisement
Takeaways from the most recent annual meeting centered around clinical advances, AI integration and professional development
Recent breakthroughs have brought attention to a previously overlooked condition
A review of treatment options for patients who may not qualify for surgery
Looking at the real-world impact and the future pipeline of targeted therapies
The progressive training program aims to help clinicians improve patient care
New breakthroughs are shaping the future of COPD management and offering hope for challenging cases
Exploring the impact of chronic cough from daily life to innovative medical solutions
How Cleveland Clinic transformed a single ultrasound machine into a cutting-edge, hospital-wide POCUS program