Case presentation, making the diagnosis and the take-home message

A 59-year-old female presented with a three-month history of worsening cervical lymphadenopathy. She reported a history of hypertension, hepatitis C and Samter’s Triad. The team performed a basic lymphadenopathy workup, which revealed elevated CRP, ESR, HCV Ab detection with undetectable viral load and a positive EBV IgG. Nephrology was consulted when her blood work showed worsening levels of her serum creatinine, from a baseline of 0.7 mg/dL to 1.2 mg/dL.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
CT imaging was obtained, revealing a potentially infiltrative pathology and enlarged cervical, mediastinal and retroperitoneal lymph nodes, including multiple bilateral renal masses with abnormal markings.
Next, a lymph node biopsy was obtained, revealing histiocytic and acute inflammatory lymphadenitis with polytypic plasmacytosis and emperipolesis. The biopsy ruled out malignancy, and immunostaining showed no infections. S-100 stained some of the histiocytes.
The patient was diagnosed with Rosai-Dorfman disease (RDD), a rare, idiopathic condition.
RDD, also known as sinus histiocytosis with massive lymphadenopathy (SHML), is not well-described in the literature. The condition is marked by the proliferation of histiocytes in lymph nodes that often occur in the neck. However, this accumulation occurs extranodally in about 40% of cases, including the skin, central nervous system, kidney and digestive tract.
RDD-associated kidney masses occur in about 4% of cases. The majority of these cases were diagnosed following a partial or radical nephrectomy, explains Moarij Qazi, MD, a nephrology fellow in Cleveland Clinic’s Glickman Urological & Kidney Institute. He presented this case in an e-poster presentation during the National Kidney Foundation’s 2021 Spring Clinical Meetings.
Once the patient was started on Prednisone 70 mg daily, her creatinine levels normalized and the infiltrates resolved.
The nephrology team recommended against a kidney biopsy, explaining that the renal abnormalities were likely a manifestation of RDD. This judicious clinical decision-making prevented surgical overtreatment and costs associated with unnecessary healthcare utilization.
Advertisement
Workup revealed kidney masses and abnormalities that were clinically concerning and potentially emblematic of a serious nephrotic syndrome or kidney cancer. However, based on the patient’s presentation, the findings of a lymph node biopsy were more revelatory than that of a kidney biopsy.
Sixteen percent of resected kidney masses are benign, says Georges Nakhoul, MD. “This is more evidence that we must maintain a high clinical suspicion when it comes to evaluating the nature of renal masses in this patient population,” he asserts.
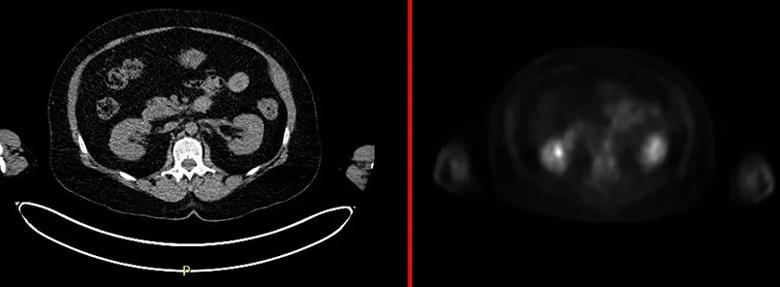
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/10145252-b616-4cbd-8bd5-b00b41a0913f/pet-inset_jpg)
Following treatment, the patient’s CT scan (left) showed resolution of masses, and the PET scan (right) did not pick up any significant hypermetabolic lesions in the kidneys.
Advertisement
Advertisement

Pediatric urologists lead quality improvement initiative, author systemwide guideline

Fixed-dose single-pill combinations and future therapies

Reproductive urologists publish a contemporary review to guide practice

Two recent cases show favorable pain and cosmesis outcomes

Meta-analysis assesses outcomes in adolescent age vs. mid-adulthood

Proteinuria reduction remains the most important treatment target.

IgA nephropathy is a relatively common autoimmune glomerular disease that can be diagnosed only by biopsy

Oncologic and functional outcomes are promising, but selection is key