Combined on-site and virtual team swiftly manages a prolonged seizure

Over the past few years, Cleveland Clinic’s Neurological Institute has dedicated substantial resources and training to the use of advanced telemedicine technologies to enhance care delivery in inpatient settings. The case study below illustrates the difference these capabilities can make in the management of inpatient emergencies.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In May 2020, a 35-year-old man with recurrent seizures was admitted to the epilepsy monitoring unit on Cleveland Clinic’s main campus to determine whether he was a candidate for epilepsy surgery.
Around 11:00 on the second night of the patient’s stay, after reduction of his epilepsy medication dosage had begun, he started to experience an aura that matched his description of the beginning of his typical seizure onset. This progressed into mouth movements and stereotypical fumbling movements of his hands. These later evolved into a generalized convulsive seizure.
The nurse on the unit followed protocol and monitored the patient’s vital signs (which were also monitored remotely by Cleveland Clinic’s central monitoring unit for cardiac telemetry) and summoned the on-site advanced practice provider (APP) who was on call for the unit. When the seizure continued for two minutes, the APP administered lorazepam, as per protocol, in an effort to end the seizure. The APP also connected by phone with technicians in Cleveland Clinic’s epilepsy central monitoring unit (ECMU), who had been remotely monitoring the patient’s EEG.
When the patient remained unresponsive three to four minutes after seizure onset, the adult medical emergency team was called to the unit in case intubation would be required to maintain breathing. Meanwhile, the ECMU technicians contacted the on-call epilepsy fellow to determine whether the seizure was still continuing or if the patient was in the post-ictal phase, as his movements were causing muscle artifacts in the EEG that were difficult to interpret.
Advertisement
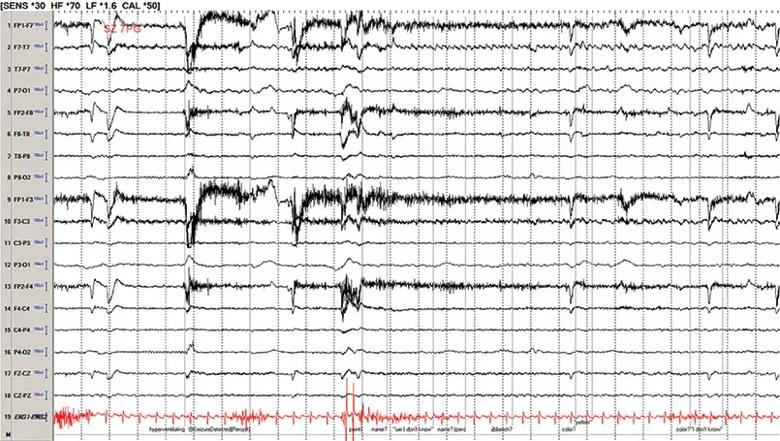
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/da5461e9-c60e-4188-9ea1-e9b84e6775df/20-NEU-1917437-CQD_EEG-seizure_inset_805x445_jpg)
A representative EEG from the patient’s seizure episode.
The epilepsy fellow was on call at home, but he was able to immediately observe the patient and speak with the on-site clinicians through two-way videoconferencing via a mobile video cart at the patient’s bedside, complete with a high-definition adjustable camera and speaker/microphone. The fellow instructed the APP to do an exam to assess for responsiveness in front of the video camera, which elicited no response other than some twitching movements.
The fellow also accessed the patient’s live video EEG via laptop computer but was not able to confirm whether the seizure was continuing or had progressed to post-ictal status, so he escalated management by calling the staff epileptologist on call, Imad Najm, MD.
Because the patient was in a unit with hardwired telemedicine capabilities in each room — i.e., a wall-mounted TV with high-definition web camera, microphone and speaker — Dr. Najm was able to immediately connect with the on-site treatment team via videoconferencing just as the fellow was doing via the mobile videoconferencing cart. Dr. Najm also accessed the patient’s live video EEG on his laptop.
Upon review of the EEG and in consultation with the fellow, the ECMU technicians and the clinicians at the bedside, Dr. Najm was able to determine that the patient was in the late post-ictal phase and that further escalation by the epilepsy and adult medical emergency teams — such as through administration of more anti-seizure medications and/or intubation and transfer to the neurological ICU — was not necessary.
Advertisement
The patient stabilized soon thereafter and was able to continue undergoing monitoring for surgical evaluation.
“This case demonstrates how new telemedicine capabilities allow us to make fully informed, highly specialized clinical management decisions for inpatient emergencies much faster than we could in the past,” notes Dr. Najm, Director of The Charles Shor Epilepsy Center, Cleveland Clinic.
“We were able to use multiple layers of technology to rapidly assemble a multidisciplinary team to appropriately manage this patient’s needs during an acute seizure event,” he continues. “We had nurses and the APP on site with the patient, along with the adult medical emergency team. We had our ECMU staff monitoring the patient’s EEG at a distance, as well as our remote cardiac central monitoring unit to monitor vital signs, which fortunately didn’t require critical action in this case. And we had both the fellow and me connecting with the management team and the patient in real time via video while we monitored the patient’s live video EEG on a second screen. Our integration of these technologies enabled bidirectional interaction with the patient and our colleagues, allowing us to base our management on the patient’s condition and brain function rather than assumptions.”
Because the telemedicine technologies gave an expert epileptologist swift and comprehensive access to all essential details of the case, the team could determine that the seizure had indeed ended and thereby avoid excessive and unnecessary interventions. Yet the team’s escalation of management to Dr. Najm was well justified, as a seizure of this type lasting more than two minutes is a red flag for potential status epilepticus or deterioration that could require intubation or transfer to the neuro ICU.
Advertisement
“Our inpatient telemedicine resources allow us to quickly and simultaneously bring together all the needed expertise and capabilities, either in person or virtually,” concludes Dr. Najm. “For an acute event of this type, this approach promotes delivery of appropriate treatment that avoids excessive care while ensuring that nothing is missed.”
Advertisement
Advertisement

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape

Study shows short-term behavioral training can yield objective and subjective gains

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits

An expert’s take on evolving challenges, treatments and responsibilities through early adulthood

Comorbidities and medical complexity underlie far more deaths than SUDEP does

Novel Cleveland Clinic project is fueled by a $1 million NIH grant

Tool helps patients understand when to ask for help