More than 6 million Americans currently suffer from congestive heart failure, and about 500,000 new cases are diagnosed each year. Despite advances in therapy, five-year mortality ranges from 40% to 50%. Though hypertension and coronary artery disease remain the primary cause, cardiac amyloidosis has been found to be the etiology with increasing frequency.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Amyloidosis is a multisystem disorder caused by the buildup of abnormal proteins in multiple organs. These proteins become misfolded, then bind together to form fibrils that circulate in the bloodstream and are subsequently deposited within the heart. As a result, cardiac failure, serious arrhythmias and cardiac death can occur without early recognition and specific therapies.
“Unfortunately, practitioner awareness of the disease has been limited and opportunities for early recognition are missed,” says David Wolinsky, MD, Section Head of Nuclear Cardiology and Director of the Cardiac Amyloidosis Center of Excellence at Cleveland Clinic Florida.
Multiple proteins are responsible for the development of amyloidosis.
Deposition of amyloid fibrils leads to marked myocardial thickening or hypertrophy of both the left and right ventricles. Though ejection fraction is preserved, diastolic dysfunction leads to HFpEF or heart failure with preserved ejection fraction with symptoms of shortness of breath and fatigue. Additionally, because of the small, stiff left ventricular cavity, cardiac output is reduced and exercise capacity becomes progressively decreased. As the disease progresses, ventricular function may worsen and ejection fraction falls, leading to worsening heart failure and quality of life.
Advertisement
Neuropathic symptoms also may be prominent. Non-cardiac symptoms such as bilateral carpal tunnel syndrome, spinal stenosis, peripheral neuropathy, and orthostatic hypotension significantly impair quality of life. “These findings are often present more than 10 years prior to the onset of cardiomyopathy but may be attributed to other diseases, delaying the diagnosis of amyloidosis,” says Dr. Wolinsky.
Most patients with amyloidosis have seen multiple cardiologists before an accurate diagnosis is made. They often have been hospitalized with signs of heart failure and fluid overload only to be readmitted shortly after discharge with recurrent symptoms. Recurrent atrial fibrillation efractory to therapy is common, as is the need for a permanent pacemaker.
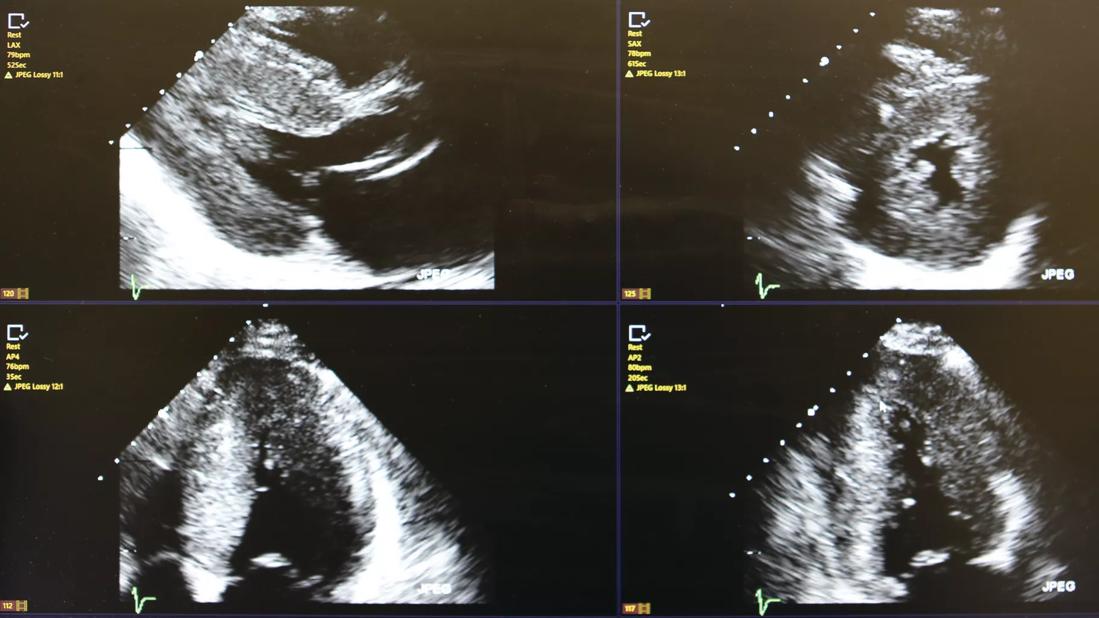
Cleveland Clinic Florida has developed a comprehensive noninvasive imaging protocol for amyloidosis evaluation. Echocardiography is an ideal screening test, demonstrating not only left ventricular hypertrophy but also typical abnormalities of the atria and valves. Most important is the performance of strain imaging as part of the standard echo protocol. This characterizes myocardial dynamics and, in amyloidosis, a characteristic pattern of “apical-sparing” can be noted. Cardiac MRI is also a useful tool as characteristic patterns of late gadolinium enhancement and the presence of increased extracellular volume may be seen.
The availability of diagnostic radionuclide imaging using bone-avid scintigraphy has dramatically increased the ability to noninvasively confirm the diagnosis of ATTR amyloidosis. Technetium pyrophosphate imaging (PYP-scanning), when done properly, can accurately diagnose ATTR amyloidosis with very high sensitivity (95% to 100%) and specificity (85% to 100%).
Advertisement
As Past-President of the American Society of Nuclear Cardiology, Dr. Wolinsky has extensive experience defining proper protocols and interpreting these scans. “I have advocated for SPECT acquisition and review for all patients. In all cases, clonal blood testing should be carried out to rule out AL amyloidosis and simple genetic testing performed to distinguish between hereditary and non-hereditary forms,” he advises.
Dr. Wolinsky also notes that scintigraphy has reduced the need for myocardial biopsy by 80% to 90%, though it is performed at the Weston Hospital campus when needed. Tissue is stained with Congo Red or Thioflavin-S for evidence of typical birefringent fibrils, and positive tissue samples are further analyzed at Cleveland Clinic’s main campus in Ohio for mass spectrometry.
Each new patient referred to Cleveland Clinic Florida’s Cardiac Amyloidosis Center undergoes an extensive initial evaluation, which includes medical history, physical exam, review of outside records and images, and discussion of further diagnostic testing and treatment plans.
“Traditional heart failure therapies such as ACE-I, ARB, and ARNI are often detrimental to amyloid patients, and the medical regimen is individualized at the first visit,” Dr. Wolinsky adds. “We discuss heart rhythm management options such as AV node ablation or cardiac resynchronization therapy and refer to our electrophysiology team if needed.”
Referrals to specialists for management of peripheral neuropathy, autonomic dysfunction, chronic spine disease, chronic kidney disease, weight loss, constipation and diarrhea also are made, when necessary. Hematology referrals are made if there is a question of the presence of AL disease. Samples for genetic testing are obtained (buccal swab) and sent out, if not already done.
Advertisement
“Because of the complexity of the initial evaluation, all our patients have the assistance of a nurse navigator throughout the process,” he says. Almost 250 patients with cardiac amyloidosis are currently being treated at the Cardiac Amyloidosis Center of Excellence.
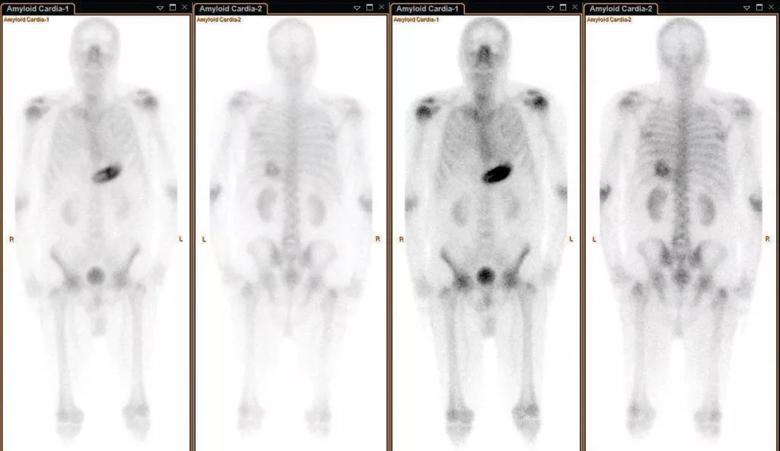
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e48f7d71-c987-499b-b44a-3608e7fdcb7f/Wolinsky_Capture3-1024x592_jpg)
Full-body planar scan demonstrating no myocardial uptake of Tc-Pyp. For totally normal planar studies, SPECT imaging may not be needed. This scan also identifies artifacts that could interfere with accurate scan interpretation.
Beyond instituting traditional heart failure therapy, patients are assessed for disease-modifying therapy at their initial visit. Transthyretin is a normally existing tetramer protein that, in amyloidosis, becomes unstable and separates into four monomers. Disease-modifying therapy is focused on either blocking the production of the unstable proteins (silencers) or preventing dissociation of the tetramer (stabilizer).
For wild-type cardiomyopathy, a stabilizer called tafamidis is often used. Cleveland Clinic Weston Hospital’s pharmacy works with patients to obtain insurance coverage for the drug, a capsule that is taken once a day and has minimal side effects. Long-term use of the drug is associated with improved survival at 18 months and 30 months, and less clinical deterioration at six months, compared to patients not on the drug.
For patients with hereditary ATTR who have peripheral neuropathy, with or without cardiac involvement, several silencers are approved to block the mRNA from producing transthyretin protein. While patients with AL amyloidosis may receive care that includes state-of-the-art treatments and access to clinical research protocols through Cleveland Clinic Florida’s Department of Hematology.
Advertisement
“Many patients with advanced AL and hereditary ATTR disease continue to deteriorate despite aggressive therapy,” observes Dr. Wolinsky. “Appropriate patients are evaluated for organ transplant including heart, liver, combined heart-liver and combined heart-kidney transplant. Our transplant team is experienced in carrying out en-bloc heart-liver transplantation, with markedly reduced surgical times and outcomes equivalent to single-organ transplantation.”
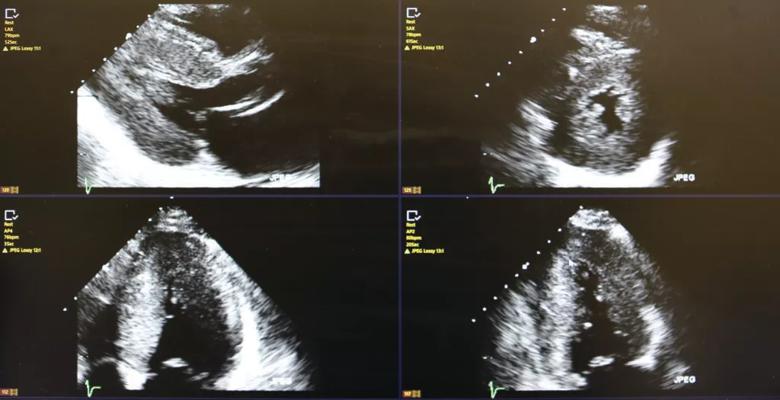
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/2de731b0-128d-4bb5-a5ff-30beb673837f/Wolinsky_9U7A2494-1024x525_jpg)
Echocardiogram demonstrating left ventricular hypertrophy and typical bright speckled appearance. Though very suggestive of ATTR cardiac amyloidosis, it is not sufficient. Only myocardial biopsy or positive pyrophosphate scan may confirm the diagnosis.
Dr. Wolinsky and his colleagues are involved in clinical research trials and the development of clinical protocols for patients who are not candidates for traditional treatment options, who cannot afford treatment options, or who have failed standard therapy. Additionally, the team is studying populations who appear to be at risk for cardiac amyloidosis, such as patients with aortic stenosis undergoing TAVR and SAVR. “South Florida is unique in its elderly population, and we are studying the natural history and response to disease-modifying therapy in the octogenarian population,” says Dr. Wolinsky, noting most cardiac amyloidosis studies involve patients with an average age of 70 to 75. “We’re also working on multiple educational initiatives to increase the clinical recognition and clinical suspicion for cardiac amyloidosis.”
Advertisement

Nonthermal technique reduces bleeding and perforation risk

Standardizing a minimally invasive approach for Barrett’s Esophagus and Esophageal Cancer

PSMA-targeted therapy for metastatic prostate cancer now offered at Cleveland Clinic Weston Hospital

Nationally recognized urologic oncologist offers vision for growth, innovation, and excellence

Noninvasive modality gains ground in United States for patients with early-to-moderate disease

Cleveland Clinic Weston Hospital’s collaborative model elevates care for complex lung diseases

Interventional pulmonologists at Cleveland Clinic Indian River Hospital use robotic technology to reach small peripheral lung nodules

Trained in the use of multiple focal therapies for prostate cancer, Dr. Jamil Syed recommends HIFU for certain patients with intermediate-risk prostate cancer, especially individuals with small, well-defined tumors localized to the lateral and posterior regions of the gland.