Nonthermal technique reduces bleeding and perforation risk
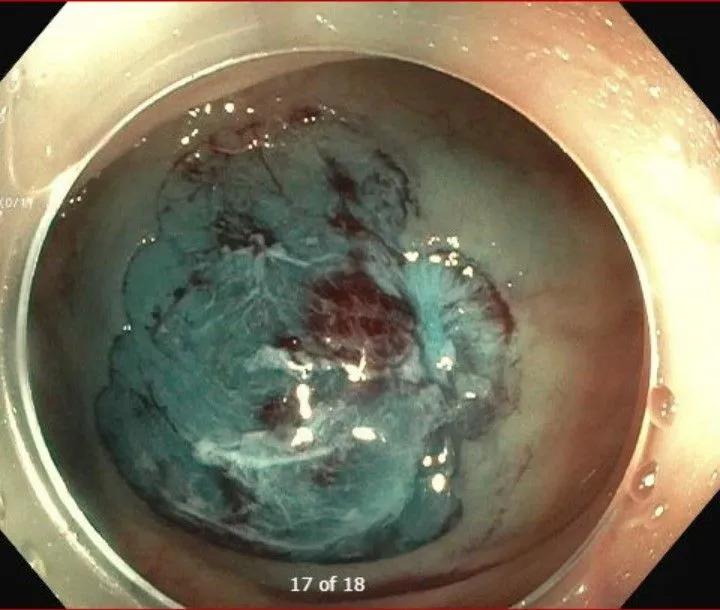
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c1208cdd-7b92-47ba-8908-9a0dd73ef0a9/Cold-EMR-After)
Cold EMR (After)
Endoscopic mucosal resection (EMR) is the standard of care for many benign colorectal lesions, offering patients a less invasive alternative to surgery. However, conventional hot EMR carries a well-recognized risk of adverse events, including delayed bleeding and perforation – complications that remain a source of concern, particularly for large polyps.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Cold EMR, which avoids electrocautery, has emerged as a compelling safety-focused alternative. Once limited to smaller lesions, it is increasingly being applied to larger and more complex polyps as experience and technique evolve. At Cleveland Clinic Weston Hospital, the interventional endoscopy team led by Tolga Erim, DO, is helping define the expanding role of cold EMR through high-volume clinical practice, education, and research.
As an advanced endoscopist, Dr. Erim is nationally recognized for his expertise in complex polyp resection and has led courses on best practices in cold EMR. He serves as Florida Division Chair of the Department of Gastroenterology, Hepatology and Nutrition and Florida Region Director of Endoscopy at Cleveland Clinic in Florida. He also holds the Lynda and Marlin Younker Endowed Chair in Developmental Endoscopy.
Cold EMR involves submucosal injection to lift a lesion followed by snare resection without electrocautery. Historically, cold techniques were limited to polyps smaller than 10 mm. Advances in technique and operator experience have expanded its use to larger lesions, although cold EMR remains an advanced approach not yet widely available.
The primary advantage of cold EMR is its safety profile. By eliminating thermal injury, the technique substantially reduces the risks of delayed bleeding and perforation, two of the most concerning complications of endoscopic resection.
This benefit has been demonstrated in multiple studies, including the first randomized, multicenter trial comparing cold snare EMR with hot snare EMR for large (≥20 mm), nonpedunculated colorectal polyps. In that study, perforation occurred in 0% of patients undergoing cold EMR compared with 3.9% in the hot EMR group (P = .007). Postprocedural bleeding was also significantly lower with cold EMR (1.0% vs 4.4%, P = .040).
Advertisement
However, efficacy remains an important consideration. The same trial demonstrated a higher rate of residual adenoma following cold EMR (23.7% vs 13.8%). Based on these findings and post hoc subgroup analyses, the investigators emphasized that “not every lesion is equally suitable for cold snare EMR.”
Clinical experience at Cleveland Clinic Weston Hospital mirrors these findings. Over the past five years, fewer than 1% of patients undergoing cold EMR at the institution have experienced delayed bleeding, and no perforations have been reported, according to Dr. Erim.
Beyond safety, cold EMR offers procedural advantages, including reduced procedure time and lower cost. “Cold resection does not require defect closure or the use of expensive clips,” he notes.
These benefits must be weighed against the risk of recurrence, making careful patient and lesion selection essential. “I will not use cold EMR alone in areas of severe scarring or submucosal fibrosis, where complete resection may be compromised,” says Dr. Erim.
He also notes that large polyps greater than 2 cm with complex morphology or those located in technically challenging areas, such as within diverticula or on folds, can also be difficult to resect. For some cases, Dr. Erim may use hot avulsion to address difficult-to-snare or fibrotic residual tissue. This adjunctive technique combines mechanical traction with short bursts of electrocautery using hot biopsy forceps.
“Hot avulsion minimizes the risk of deep thermal injury seen with hot snare methods and may help minimize polyp recurrence,” he explains.
Advertisement
Weston Hospital is actively investigating endoluminal resection techniques. A large retrospective study conducted in collaboration with researchers at the University of Florida compares cold EMR with hot EMR for the removal of large, complex polyps. The study includes 764 patients treated between 2010 and 2022, with results expected later this year.
In addition, the team has launched an investigator-initiated, randomized, non-blinded clinical trial evaluating a hybrid EMR strategy for large (≥20 mm) polyps. In the intervention arm, lesions will be removed via cold EMR, followed by hot avulsion of any visible residual neoplasia within the resection bed. At the endoscopist’s discretion, targeted argon plasma coagulation (APC) may be applied to ablate microscopic residual tissue at the resection bed and margins.
The control group will undergo cold EMR with cold forceps removal of visible residual tissue that cannot be ensnared. Primary outcomes will include recurrence rates and adverse events such as perforation, bleeding, and post-polypectomy syndrome.
In current practice, cold EMR is preferred for smaller, non-dysplastic polyps (10-19 mm) because of the lower bleeding risk. It is also used for carefully selected larger (≥20 mm) sessile serrated lesions and certain flat adenomas. Hot EMR remains preferred for high-risk lesions or those with deep invasion or fibrosis, where cold snare resection may increase recurrence risk.
These practice patterns align with the latest guidelines on endoscopic removal of colorectal lesions from the U.S. Multi-Society Task Force on Colorectal Cancer and the more recent clinical practice update from the American Gastroenterological Association.
Advertisement
Despite the safety and cost-effectiveness of EMR compared with surgery, research indicates an increasing use of colectomy for benign colorectal lesions. Dr. Erim emphasizes that appropriate referral is critical to reversing this trend. Patients with endoscopically resectable polyps should be referred to centers with advanced endoscopists experienced in complex resection techniques.
“Endoscopic resection allows patients to avoid surgery and preserve quality of life,” he adds.
Use of EMR itself is becoming more common. One study reported an increase in EMR use in the United States from 1.62% of all colonoscopies in 2011 to 2.48% in 2015 (P < .001). Given that approximately 15 million colonoscopies are performed annually in the U.S., even incremental improvements in technique, safety, and patient selection can have a substantial impact.
Through clinical leadership, education, and a robust research agenda, Dr. Erim and his team at Cleveland Clinic Weston Hospital are helping define best practices in cold EMR – advancing safer, less invasive options for patients while refining the evidence base for endoscopists nationwide.
Advertisement
Advertisement
Standardizing a minimally invasive approach for Barrett’s Esophagus and Esophageal Cancer
PSMA-targeted therapy for metastatic prostate cancer now offered at Cleveland Clinic Weston Hospital
Nationally recognized urologic oncologist offers vision for growth, innovation, and excellence
Noninvasive modality gains ground in United States for patients with early-to-moderate disease
Cleveland Clinic Weston Hospital’s collaborative model elevates care for complex lung diseases
Interventional pulmonologists at Cleveland Clinic Indian River Hospital use robotic technology to reach small peripheral lung nodules
Trained in the use of multiple focal therapies for prostate cancer, Dr. Jamil Syed recommends HIFU for certain patients with intermediate-risk prostate cancer, especially individuals with small, well-defined tumors localized to the lateral and posterior regions of the gland.
Cleveland Clinic Weston Hospital is actively recruiting patients for an international, multicenter, phase III study comparing MIS versus open interval cytoreduction following neoadjuvant chemotherapy in patients with stage IIIC-IV epithelial ovarian cancer.