Retired-protein strategy represents new approach to immunization

Cleveland Clinic has begun clinical testing of a novel vaccine designed ultimately to prevent triple-negative breast cancer (TNBC) by priming high-risk women to mount an immune response against a “retired” lactation protein expressed only in cancer cells.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
TNBC is so-named because patients’ cancer cells test negative for estrogen and progesterone receptors and the human epidermal growth factor receptor 2 (HER2) protein, making hormone therapy and HER2-targeted drugs ineffective. It accounts for 12-15% of all breast cancers and is the most aggressive and lethal subtype. Nearly one-quarter of all TNBC patients die within five years of diagnosis; five-year survival in patients with distant metastases is only 12%. TNBC disproportionately affects Black women and women with germline BRCA1 gene mutations. The only effective prophylaxis currently available to women at high risk for TNBC is bilateral mastectomy.
The prototype Cleveland Clinic vaccine represents a potential new way to combat breast cancer. It is the result of nearly two decades of research by immunologist Vincent Tuohy, PhD, of the Lerner Research Institute’s Department of Inflammation and Immunity. Dr. Tuohy persevered despite others’ skepticism about his unusual approach and the difficulty of obtaining funding to support years of basic science work to determine the vaccine’s feasibility.
“There was a lot of resistance to these kinds of new ideas,” he says. “It took a long time for people to think that this vaccine wasn’t just pie in the sky — that it was based on good science and was doable.”
Dr. Tuohy is the primary inventor of the vaccine technology, which Cleveland Clinic has licensed to Anixa Biosciences, Inc. He will receive a portion of commercialization revenues received by Cleveland Clinic for this technology and also holds personal stake in the company.
Advertisement
The U.S. Food and Drug Administration recently approved an investigational new drug application for the vaccine, allowing the clinical trial to move forward. The study is funded by the U.S. Department of Defense.
Most breast cancer vaccines presently in development are meant to treat patients with existing tumors or to prevent recurrence in cancer survivors.
Current data indicate that therapeutic vaccines have limited efficacy, at least in part because they employ target antigens that fail to induce a clinically relevant immune response and adjuvants that don’t adequately enhance the response. Only one breast cancer vaccine has progressed to phase III trials, and that randomized trial was terminated for futility when interim analysis showed no difference in disease-free survival between the vaccine and placebo.
Dr. Tuohy’s experimental vaccine is aimed at primary prevention – stopping cancer before tumors develop.
“We know from the childhood vaccine program that vaccines are to prevent disease,” he says. “You don’t wait to get polio or measles and then vaccinate. But the entire field of cancer vaccination was using vaccines to treat. And I thought that wasn’t right. As a standalone, therapeutic cancer vaccines have not worked well,” primarily because of the tumors’ substantial head start in growth, the onset of clinical symptoms, the establishment of tumor defenses against the immune response, and the potential for local and distant metastasis.
The experience Dr. Tuohy gained developing a new animal model of multiple sclerosis and studying self-recognition and autoimmune diseases sparked his interest in harnessing autoimmunity to preemptively attack nascent cancer cells.
Advertisement
The difficulty with that approach is that potential tumor antigens are variations of normal self-generated molecules. A prophylactic cancer vaccine targeting such antigens likely would trigger profound, systemic autoimmune complications.
To avoid that problem, Dr. Tuohy sought to target tissue-specific proteins that were no longer expressed in normal tissues because of the aging process but were expressed in tumors that emerge with age, such as breast, ovarian and prostate cancers. He called this idea the retired protein hypothesis.
In breast tissues, many proteins dedicated to lactation are no longer expressed – in essence, retired – after a woman exceeds child-bearing age. Employing a retired lactation protein as a breast cancer vaccine autoantigen made sense because most breast cancers occur in women ages 40 and older, and the vast majority of those women no longer breastfeed.
Dr. Tuohy and his research team chose the breast-specific lactation protein α-lactalbumin as their target vaccine autoantigen because it is no longer found in detectable amounts in normal, aging breast tissues but is expressed at high levels in more than 70% of TNBCs. They verified its expression in human TNBC tissues using molecular and immunohistochemical analyses.
The reason for α-lactalbumin expression in TNBC tumors is unclear but may be due to the lack of estrogen and progesterone receptors, which otherwise would facilitate inhibition of α-lactalbumin transcription. “Tumors do bizarre things,” Dr. Tuohy says. “Expressing α-lactalbumin is a mistake that the TNBC tumors make, and we’re taking advantage of this mistake.”
Advertisement
Among the concerns Dr. Tuohy and his team sought to address: Whether adult women would immunologically respond to α-lactalbumin; whether prior lactation would create an insurmountable tolerance that precluded generating effective immunity against α-lactalbumin; and whether expression of α-lactalbumin in normal nonbreast tissues would cause systemic autoimmune complications.
The researchers first showed that immunizing mice with a single injection of whole recombinant mouse α-lactalbumin provided significant protection against tumor formation and growth in several mouse models for breast cancer. The level of protection was virtually identical in parous mice with a history of lactation and breastfeeding and in nonparous mice with no lactation history.
Next, the investigators demonstrated that nonlactating mice immunized with α-lactalbumin showed no autoimmune inflammatory damage.
“We found that the animals developed tumor immunity without autoimmunity, and that was the secret to moving forward with our concepts,” Dr. Tuohy says. The findings bolstered the team’s belief that α-lactalbumin vaccination could safely and effectively protect healthy women against developing TNBC. They began planning phase I clinical trials to provide safety and dosage profiles and determine the number of vaccinations needed for inducing optimum immunity.
Video content: This video is available to watch online.
View video online (https://www.youtube.com/embed/sVvLTiRRKgo?feature=oembed)
Breast Cancer Vaccine | How Does it Work?
The selection of the adjuvant component for the preventive vaccine was critical, both in terms of its ability to activate the aggressive proinflammatory T-cell response needed for effective tumor immunity, and to pass regulatory scrutiny. Adjuvants are necessary to activate the innate immune response for orchestrating the adaptive immune response and conferring immunological memory.
Advertisement
“The adjuvant is the irritant,” Dr. Tuohy says. “It provides the danger signal. So now the immune system sees α-lactalbumin in the context of a danger signal and activates the entire cascade of innate and adaptive immunity.”
Dr. Tuohy and his colleagues tested multiple adjuvants that proved to be inferior before developing a weakened version of complete Freund’s adjuvant (CFA).
CFA — desiccated mycobacterium suspended in mineral oil — is a potent anti-inflammatory agent whose use in humans is prohibited and in research animals is limited due to its toxicity and potential to cause granulomas and abscesses.
“We used a lighter oil and, instead of mycobacteria, we used the wall of a yeast, which is slightly less immunogenic but still sufficient to elicit a broad immune response,” Dr. Tuohy says. “By that, I mean an inflammatory T-cell response that produces interferon-gamma and interleukin-17. We want to create a florid inflammatory response capable of destroying a tumor as it emerges. We think that many cancer vaccines haven’t worked because they used weak adjuvants. We believe our adjuvant is the most potent adjuvant used in a human cancer vaccination.”
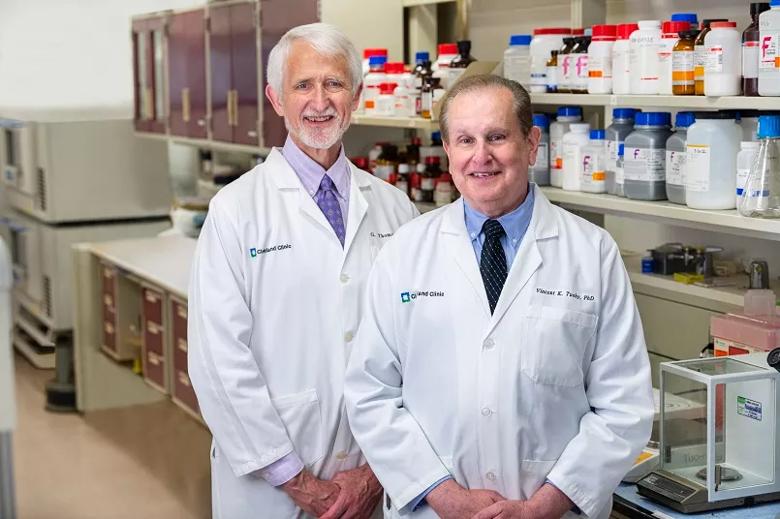
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/eb76d15b-3bb1-4c3e-83ee-8012f8548f4b/21-CCC-2313409-Breast-cancer-vaccine-Budd-and-Tuohy-805x450-1_jpg)
G. Thomas Budd, MD, (left) is the breast cancer vaccine trial’s principal investigator and Vincent Tuohy, PhD, is the vaccine’s primary inventor.
Because the new vaccine’s safety and clinical benefit have not been established in humans, it would be ethically problematic for its initial prevention trial to involve TNBC-at-risk but otherwise healthy women as recipients.
Therefore, the phase I dose-escalation trial will enroll approximately 24 women who are within three years of TNBC diagnosis and currently have stable disease with high risk of recurrence.
“These are patients who may have microscopic cancer cells present in their body, so a vaccination when the disease is microscopic could provide some benefit,” says Cleveland Clinic oncologist G. Thomas Budd, MD, the trial’s principal investigator. “Long-term, we are hoping that this can be a true preventive vaccine which would be administered to healthy women and prevent them from developing triple-negative breast cancer, the form of breast cancer for which we have the least effective treatments.”
In the current trial, participants will receive up to three vaccinations, each two weeks apart, to determine the optimal immunologic dose and the maximum tolerated dose. The women will be closely monitored for side effects and immune response, the latter assessed by blood tests to detect a pro-inflammatory T cell response consistent with tumor protection. The study is expected to be complete in September 2022.
If the initial trial confirms the vaccine’s safety and its ability to produce an effective immune response in post-therapy, disease-free TNBC patients, subsequent trials would similarly test it in women who are at high risk for TNBC but have not yet developed the disease.
“I think we can anticipate early trials in women with BRCA1 mutations in the next two to four years,” Dr. Budd says. “These would be nonrandomized trials, looking for a signal of effectiveness and for side effects that may be less common than those we might identify in the early, small trials. It will be a number of years before we can do randomized trials where we vaccinate half the patients and give the other half a placebo. And it will be even more years before we can broaden the patient population to women outside of these very high-risk groups.
“There are potential hurdles along the way,” Dr. Budd says, “but I’m optimistic that we can overcome those and help women who are at risk for breast cancer. I think we can tell women now that there is hope for their children and grandchildren.”
Dr. Tuohy is hopeful the retired-protein strategy will enable vaccines that prevent other types of cancers in addition to TNBC.
He is developing an ovarian cancer vaccine that targets the extracellular domain of anti-Müllerian hormone receptor II (AMHR2-ED), an ovary-specific self-protein. AMHR2-ED plays a role in fetal sex development and, in premenopausal women, it helps regulate ovarian reserve and fertility. Its presence declines to nonautoimmune-inducing levels in postmenopausal ovaries, but it is expressed in approximately 90% of epithelial ovarian carcinomas (EOC), the most prevalent and lethal form of ovarian cancer.
Dr. Tuohy’s preclinical research using a mouse model of EOC has shown that AMHR2-ED vaccination significantly inhibits tumor growth and improves overall survival without inducing autoimmune oophoritis in aged female mice. He has a collaboration agreement with the National Cancer Institute’s PREVENT preclinical drug development program to develop this vaccine for use in preventing EOC and endometrial cancer, which also expresses AMHR2-ED in many cases.
Dr. Tuohy believes a similar approach is possible for preventing prostate cancer and other cancers that appear as adults age.
“There is a great need for a 21st-century vaccine program that protects us from diseases we confront with age, in the same way that 20th-century vaccines protected us from childhood infectious diseases,” Dr. Tuohy says. “I envision our efforts at Cleveland Clinic being the beginning of that. This is the first step of many, many steps. I won’t be around for all of them, but we’re not done until we eliminate all of these different cancers.”
Advertisement

First full characterization of kidney microbiome unlocks potential to prevent kidney stones

Researchers identify potential path to retaining chemo sensitivity

Large-scale joint study links elevated TMAO blood levels and chronic kidney disease risk over time

Investigators are developing a deep learning model to predict health outcomes in ICUs.

Preclinical work promises large-scale data with minimal bias to inform development of clinical tests

Cleveland Clinic researchers pursue answers on basic science and clinical fronts

Study suggests sex-specific pathways show potential for sex-specific therapeutic approaches

Cleveland Clinic launches Quantum Innovation Catalyzer Program to help start-up companies access advanced research technology