Correlation of systemic disease, urologic symptoms confirmed

Cleveland Clinic’s Department of Urology created the Center for Men’s Health last year to help improve the care of men with urologic conditions by bringing together urologists, cardiologists and endocrinologists, among others.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Key to the center’s approach is a new men’s health phenotype that it developed based on the hypothesis that there is a correlation between total burden of systemic disease and severity of urologic symptoms. Bearing the acronym A-C-T-I-O-N-S, the phenotype classifies men according to presence and severity of seven conditions:
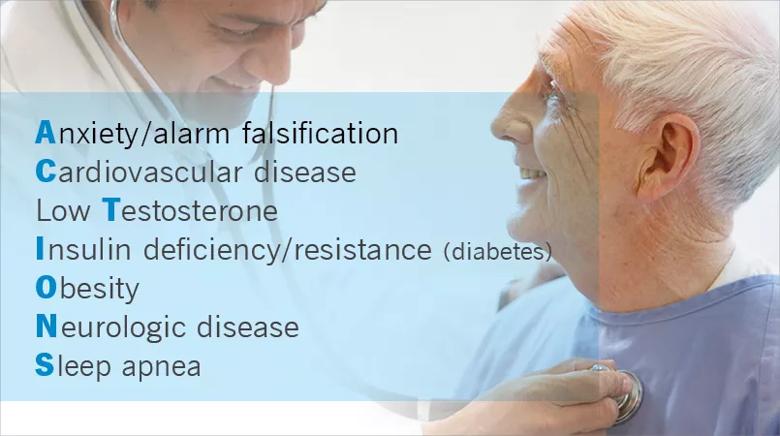
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/3399fddf-a2be-413f-9def-0c87bf9b990c/805x-Inset-ACTIONS_jpg)
The greater the systemic comorbidity burden, the less likely that specific urologic interventions are likely to succeed, the team believes.
This phenotype has now been validated by retrospective chart review study published recently in Urology.
In the study, 4,258 men who sought care for benign prostatic hypertrophy (BPH), erectile dysfunction (ED) or chronic pelvic pain syndrome (CPPS) over the past seven years were identified for possible review. Patients were excluded if the chart did not have complete information about the urologic or systemic conditions of interest, which brought the total down to 1,139 patients.
A priori sample size calculation suggested a minimum of 400 patient records be used to show a correlation between all variables. To ensure minimal representation of potentially under-represented groups, blocks were created based on age, urologic diagnosis, and body mass index. Charts were ordered by medical record number within these blocks and 415 overall were randomly selected for analysis.
Each patient’s urologic condition was graded as absent or mild (rated as 0), moderate (rated as a 1) or severe (rated as a 2), according to accepted guidelines including International Prostate Symptom Score, the Sexual Health Inventory for Men and National Institute of Health Chronic Prostatitis Symptom Score. They were tallied to achieve an overall Urologic Score (US). The seven systemic conditions of the ACTIONS phenotype were similarly graded to arrive at a Systemic Score (SS).
Advertisement
Two hundred-forty patients (58 percent) were found to have one urologic condition of at least moderate severity, 19 (32 percent) had two and 28 (7 percent) had all three. The rest had a chief complaint of BPH, ED or CPPS but of less-than-moderate severity. The mean total US was 2.1 (range 0-6) and mean SS was 4.1 (0-12).
“We found a strong and consistent correlation between total US and SS across all age groups,” says Sarah C. Vij, MD, of Cleveland Clinic’s Glickman Urological & Kidney Institute and one of the study co-authors.
The greatest impact was seen in patients who had cardiovascular comorbidities, followed in declining order by neurologic problems, diabetes, anxiety, sleep apnea, obesity and low testosterone.
Dr. Vij says that these findings validate the team’s belief that systemic diseases contribute considerably to urologic disorders. Treatments directed at the genitourinary system alone may not make a significant impact on the patient’s burden of symptoms, which supports the need for a Center for Men’s Health that aims to treat the patient as a whole.
“In what we believe to be the first comprehensive analysis of its kind, we have demonstrated that systemic health conditions correlate strongly with urologic symptoms in men who present for urologic care. Our original men’s health phenotype, ACTIONS, appears to meet the standards of being a useful and practical instrument for clinicians treating this population,” she says.
As the ACTIONS phenotype is further validated, Dr. Vij notes, the US might become an accepted tool to determine the need to screen patients for specific systemic conditions.
Advertisement
“This would further increase the phenotype’s impact on improving men’s overall health,” she says.
Dr. Vij mentions several drawbacks to the study. One is that it was performed at a single time point, which does not allow for analysis of bidirectional causality or degree of improvement in urologic symptoms.
Also, since the systemic scores were based on conditions diagnosed in the past, researchers were unable to assess their current impact or ensure consistency in diagnostic criteria. In addition, the systemic score system is not a validated scoring system.
Future prospective, community-based studies are needed to further validate these findings, but Dr. Vij says the overall message of this study is that there is now a demonstrated direct correlation between presence and severity of systemic conditions and BPH, ED and CPPS.
“The use of the ACTIONS phenotype can be useful in educating patients, informing treatment decisions and ultimately improving urologic and overall health outcomes, having a significant impact on our patients’ quality of life,” she says.
Advertisement
Advertisement

Pediatric urologists lead quality improvement initiative, author systemwide guideline

Fixed-dose single-pill combinations and future therapies

Reproductive urologists publish a contemporary review to guide practice

Two recent cases show favorable pain and cosmesis outcomes

Meta-analysis assesses outcomes in adolescent age vs. mid-adulthood

Proteinuria reduction remains the most important treatment target.

IgA nephropathy is a relatively common autoimmune glomerular disease that can be diagnosed only by biopsy

Oncologic and functional outcomes are promising, but selection is key