Study reviews institutional experience
Limited information is available about urosymphyseal fistula (USF), a rare malformation associated with severe pelvic pain, chronic opioid use, and typically occurring in patients who have received radiotherapy for a pelvic malignancy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
This prompted a team of urologists at Cleveland Clinic to lead an institutional review of USF cases to better understand the condition, outline treatment approaches, and raise awareness about it within the field. They published their findings in European Urology Focus.
Kenneth Angermeier, MD, urologist and lead author of the study, says patients with USF usually report recurrent urinary tract infection, pelvic pain, hematuria, and have commonly undergone prior radiation therapy for prostate cancer or as neoadjuvant therapy.
“Many have severe pelvic pain and even trouble ambulating, and this really impacts their quality of life. We wanted to see how much treatment impacted the use of opioids in their pain control,” he says.
Their study included data from 33 patients treated at Cleveland Clinic over a 12-year period (2009-2021). The key findings include:
Most patients received radiation therapy. 94% of the patients studied had a history of brachytherapy or external beam radiation therapy for pelvic malignancy. USF was diagnosed at a median of 11 years after cancer treatment, often following endoscopic procedures for bladder outlet obstruction.
More than 80% of cases of USF occurred from 2016 to 2021, which suggests a more recent uptick in cases. This raises concerns that incidence of the condition may be increasing, which could be a result of more aggressive radiotherapy regimens for prostate cancer treatment; alternatively, these data may reflect improved detection and awareness of USF.
Advertisement
Infection is commonly involved. Osteomyelitis, infection of the pubic bone, was suspected in about 80% of the imaging reports reviewed, and urine cultures were commonly positive preoperatively.
All patients were managed surgically. More than 90% underwent cystectomy with ileal conduit urinary diversion, pubic bone debridement or resection, followed by placement of an omental pedicle flap into the pelvis. Certain patients may be managed with a bladder-sparing operation, but candidates for this approach are uncommon.
Dr. Angermeier adds, “The vast majority of these patients will need a cystectomy, and they will also need to have their pubic bone debrided or resected as well to prevent ongoing abscesses and infection-related complications after the surgery.”
Pain scores decreased significantly postoperatively, from a 4 (IQR0–8) to 0 (IQR0) (p < 0.001), enabling many patients to cut down on their pain medication or discontinue use altogether. Chronic opioid use decreased from 39.4% to 21.2% (p = 0.02).
“Often patients will report significantly improved pelvic pain even while they’re still recovering from the procedure in the hospital,” says Dr. Angermeier, “it only takes a couple of days.”
“Now that we’ve seen a fair number of these cases, when someone presents with those symptoms and that history, we can almost always anticipate a USF diagnosis, which we can then confirm with an MRI of the pelvis,” says Dr. Angermeier.
He hopes this study and others like it will increase suspicion of the condition among urologists.
Advertisement
“If your patient has a medical history of radiation for prostate cancer and is experiencing the classical symptoms of USF, consider this diagnosis, confirm it with an MRI, and refer to a specialist if needed—the earlier it’s managed, the better. Surgical intervention can significantly improve pain, decrease the risk of chronic opioid use, and improve quality of life.”
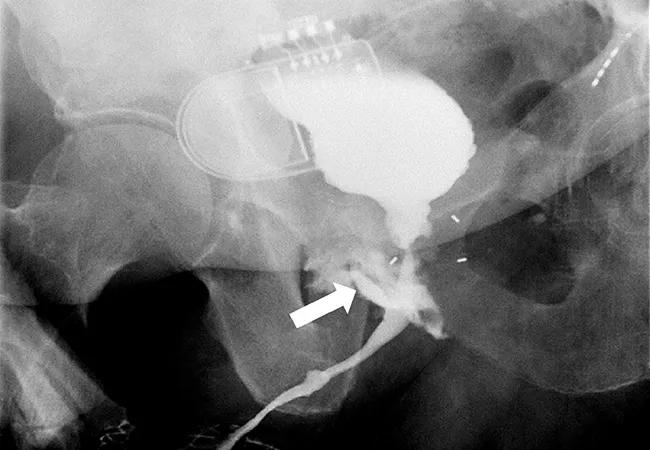
Featured image: Imaging showing urosymphyseal fistulas.
Reprinted from Anele UA, Wood HM, Angermeier KW. Management of Urosymphyseal Fistula and Pelvic Osteomyelitis: A Comprehensive Institutional Experience and Improvements in Pain Control. Eur Urol Focus. 2021 Aug 31:S2405-4569(21)00223-6. doi: 10.1016/j.euf.2021.08.008. with permission from Elsevier.
Advertisement
Advertisement

Pediatric urologists lead quality improvement initiative, author systemwide guideline

Fixed-dose single-pill combinations and future therapies

Reproductive urologists publish a contemporary review to guide practice

Two recent cases show favorable pain and cosmesis outcomes

Meta-analysis assesses outcomes in adolescent age vs. mid-adulthood

Proteinuria reduction remains the most important treatment target.

IgA nephropathy is a relatively common autoimmune glomerular disease that can be diagnosed only by biopsy

Oncologic and functional outcomes are promising, but selection is key