Nephrologists discuss the most recent practice guidelines

By Ali Mehdi, MD, MEd; Jonathan J. Taliercio, DO; and Georges Nakhoul, MD, MEd
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Contrast-induced acute kidney injury (CI-AKI) is one of the most feared adverse effects of iodinated contrast media for computed tomography (CT). Newer and safer contrast agents and, perhaps, better patient selection and prophylactic measures have ameliorated those risks. Recently, some authors have questioned whether CI-AKI is an actual entity.
This review presents and evaluates the data around CI-AKI and highlights the most recent practice guidelines.
Iodinated contrast media are commonly used in modern medicine both intravenously with CT studies and arterially during angiographic procedures. Among the possible adverse effects is acute kidney injury (AKI), first reported in the 1950s in patients undergoing intravenous pyelography.1 In the 1980s, larger series of cases of AKI following coronary angiography were reported, and the term contrast-induced nephropathy was coined.2 With growing attention, it was said to be one of the most common causes of hospital-acquired AKI,3 contributing significantly to incident chronic kidney disease, end-stage kidney disease and death.4
Early publications defined contrast-induced nephropathy as an increase in creatinine of 0.5 mg/dL or more, or a 25% increase from baseline within two to five days of exposure.
In 2012, the Kidney Disease Improving Global Outcomes Working Group suggested the term CI-AKI and defined it as a 50% increase in creatinine from baseline within seven days of exposure or a 0.3 mg/dL increase within 48 hours.5 CI-AKI is now the accepted terminology to describe kidney injury precipitated by iodinated contrast media.
Advertisement
CI-AKI usually presents within 24 to 48 hours of exposure to iodinated contrast media, with elevation in creatinine and, rarely, oliguria. The creatinine level peaks by three to five days and usually returns to baseline by seven to 10 days. Sediment analysis shows granular casts and tubular epithelial cells, and the fractional excretion of sodium is usually low. Risk factors include chronic kidney disease (CKD), diabetes, proteinuria, volume depletion and concomitant exposure to other nephrotoxins. Procedure-related factors include higher-osmolality contrast media, higher volume given, multiple administrations of iodinated contrast media, and intra-arterial administration with first-pass effect.2,6 The diagnosis is clinical, and it is prudent to rule out other causes of AKI, in particular, atheroembolic kidney disease in patients undergoing angiography with iodinated contrast media.7 While the true incidence of atheroembolic kidney disease compared with that of CI-AKI in this situation is not known, supporting evidence comes from reports demonstrating a correlation between the risk of AKI and atheroma burden,8 and a lower risk with radial than with femoral angiographic procedures.9 This disease has a very different clinical course but is commonly misdiagnosed as CI-AKI.
The pathophysiologic basis for CI-AKI is still not completely understood, but direct and indirect mechanisms have been suggested.10
Iodinated contrast media are directly toxic to the tubular epithelial cells, leading to loss of polarity (loss of channel restriction to either luminal or basolateral membranes) and eventual apoptosis and necrosis. Elevated blood osmolality due to the contrast media, increased viscosity of the luminal fluid and free radical formation have also been implicated in direct toxicity.7,8
Advertisement
Deranged hemodynamics underlie the indirect adverse effects of iodinated contrast media, with a brief initial vasodilatory state followed by pronounced and sustained vasoconstriction. Prolonged vasoconstriction, which appears to be mediated through alterations in endothelin, nitric oxide, adenosine, and prostaglandin levels, eventually leads to medullary ischemia. Tubuloglomerular feedback has also been postulated as an explanation for the drop in glomerular filtration rate observed in CI-AKI.
Over the past decade, a number of large epidemiologic studies suggested that AKI following exposure to iodinated contrast media is not necessarily caused by the contrast media. Some reports even questioned whether it is a real disease.11 This has sparked much debate and led to newer names for the phenomenon, including postcontrast acute kidney injury and contrast-associated acute kidney injury (Table 1). The rationale of these new definitions is to eliminate the causality associated with the term CI-AKI.
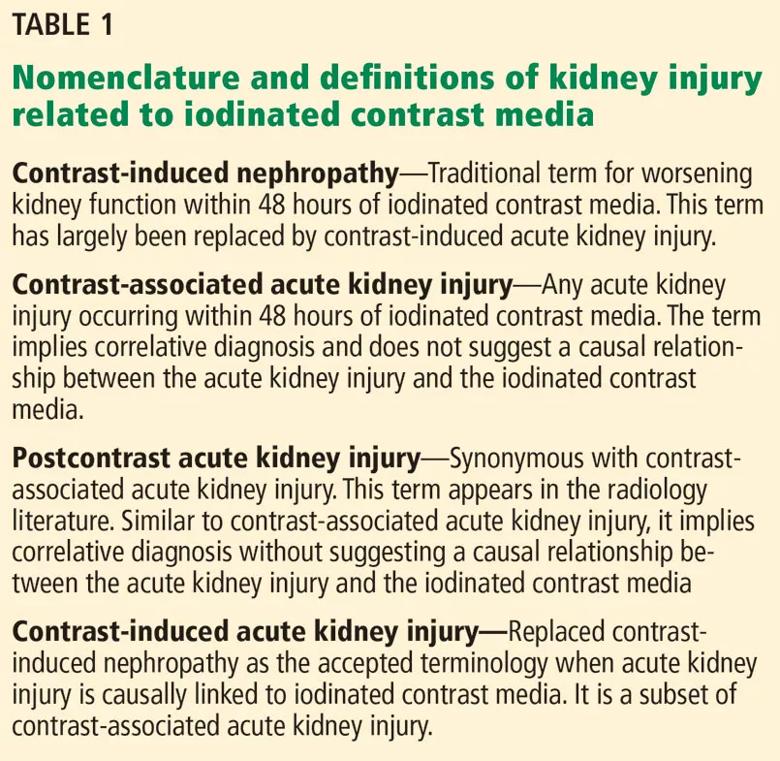
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c7ec97c0-88b1-4a56-90c1-980f71335319/805x-Table-1_jpg)
Whether one believes CI-AKI is real or a myth, this debate is not merely theoretical because conclusions drawn have significant implications for the care of our patients who have CKD. For example, Chertow et al12 reported an inappropriately low rate of cardiac angiographic procedures in patients who have CKD. Presumably, procedures were withheld out of concern for CI-AKI. They coined the term “renalism” to indicate the perhaps inappropriate attention to the kidneys while ignoring the bigger picture. Although it is not yet reported, one could presume the notion of avoidance may encompass all contrast-enhanced CT studies in the CKD population.
Advertisement
Those who question the diagnosis of CI-AKI point to studies reporting similar rates of AKI in patients undergoing contrast-enhanced CT compared with those undergoing an unenhanced study. Davenport et al13 used a 1:1 propensity matching algorithm and retrospectively reviewed over 17,000 patients who underwent contrast-enhanced CT or unenhanced CT. In patients whose estimated glomerular filtration rate (eGFR) was less than 30 mL/min/1.73 m2, the rate of AKI was significantly higher in those exposed to contrast (36.4% vs 19.4%, odds ratio 2.96, 95% confidence interval 1.22–7.17). In those with eGFRs of 30 to 59 mL/min/1.73 m2 rates were numerically higher with contrast than without contrast, but the difference did not reach statistical significance, and rates were the same with or without contrast in those with eGFRs of 60 or higher.
McDonald et al14 and, more recently, Hinson et al15 performed similar large epidemiologic propensity-controlled studies showing no difference in rates of AKI between contrast recipients and those who underwent unenhanced CT. Notably, both studies demonstrated no difference regardless of the definition of AKI or eGFR stratification. However, patients with eGFRs less than 45 mL/min/1.73 m2 accounted for only 5% to 10% of participants, with some studies completely excluding patients whose creatinine was above 4 mg/dL.15
Does that mean that CI-AKI does not exist? We believe that would be an erroneous conclusion. Despite the complex algorithms used in the propensity matching, a selection bias remains as to who undergoes contrast CT and who does not. Clinicians’ perceptions of risks and consequently their decisions to give or withhold contrast cannot be ascertained from retrospective analyses. In addition, prevention strategies, or lack thereof, are not accounted for in these large database-driven studies. Moreover, as stated previously, patients with severely decreased eGFR, who are at highest risk of CI-AKI, were less well represented in the propensity score studies.
Advertisement
However, the risks of CI-AKI are probably overstated. Initial descriptive studies were mostly uncontrolled, and rates of AKI were based mostly on ICD codes with little adjudication as to the cause. This would ultimately inflate the rates of AKI attributed to the iodinated contrast media.16,17 In addition, changing practices, such as prophylaxis, minimizing exposure, and the development of less toxic, lower-osmolar iodinated contrast media have probably played an important role in reducing the rates of CI-AKI.
Nevertheless, CI-AKI remains real. A recent meta-analysis with more than 1,500 patients undergoing peripheral angiography found a higher incidence of AKI with iodinated contrast media than with carbon dioxide contrast (11% vs 4%, respectively.18 In addition, our group recently published a propensity-matched study evaluating rates of AKI in patients with stage 3 or 4 chronic kidney disease undergoing coronary angiography, contrast-enhanced CT, or nonenhanced CT.19 Postcontrast AKI was noted in 27%, 24% and 24% of patients, respectively. All cases of AKI were then adjudicated by two nephrologists through chart review to ascertain the cause. They found that the incidence of CI-AKI was 16.5% in the coronary angiography group and 12.5% in the contrast-enhanced CT group.
Therefore, despite the lack of conclusive data, CI-AKI remains very much a real entity, although the incidence is lower than originally thought.
The evidence regarding strategies to prevent CI-AKI is far from satisfying. Hiremath and Velez16 described it as “a proliferation of small, underpowered trials, often with interventions that were poorly thought out” and said that “subsequent meta-analyses have spawned meta-confusion.” With that in mind, we will try to critically evaluate some of the proposed prophylactic interventions.
Solomon et al20 first reported volume expansion with 0.45% saline to be effective in preventing CI-AKI. Mueller et al,21 analyzing 1,620 patients, reported a lower incidence of AKI with periprocedural use of isotonic saline than with 0.45% saline.
Although hydration has become the accepted standard, the recent AMACING trial challenged its role in preventing CI-AKI. Nijssen et al22 randomized 660 patients undergoing contrast-enhanced procedures to undergo volume expansion with 0.9% normal saline or no volume expansion. The latter was found to be non-inferior to saline, but the overall rates were low. Notably, patients with an eGFR less than 30 mL/min/1.73 m2 were excluded from the study.
More recently, Timal et al23 performed a randomized multicenter trial in 523 patients with stage 3 CKD undergoing contrast-enhanced CT. Randomization to no hydration was non-inferior to prehydration with bicarbonate in terms of postcontrast AKI, with event rates of 2.7% vs 1.5% respectively (relative risk 1.7, 95% CI 0.5–5.9). Noninferiority was also shown on subgroup analyses based on age, eGFR (30–44 vs 45–60 mL/min/1.73 m2) alone or in combination with risk factors including diabetes. However, the event rate in this trial was lower than in previous trials, and therefore, caution should be used with interpreting the results.
The type of fluid used for volume expansion has also been a topic of debate, with bicarbonate-based hydration protocols proposed. The premise is that urinary alkalinization would ameliorate the direct toxicity of iodinated contrast media by decreasing oxygen free-radical generation.10
Multiple small trials and subsequent meta-analyses provided highly divergent results until the Prevention of Serious Adverse Events Following Angiography (PRESERVE) trial put this discussion to rest.24 This large 2-by-2 factorial study randomly assigned 5,177 patients undergoing nonemergency angiography to receive isotonic sodium bicarbonate vs isotonic saline as well as oral acetylcysteine vs placebo. The trial was stopped early due to futility, with AKI rates of 9.5% in the bicarbonate group and 8.3% in the saline group (P = .13). Therefore, there is no additional benefit to bicarbonate-based hydration compared with isotonic saline.
Acetylcysteine. The acetylcysteine story mirrors that of bicarbonate: a multitude of small studies followed by a series of meta-analyses yielding conflicting results. However, two studies over the past few years should settle this discussion for good: the Coronary and Peripheral Vascular Angiography (ACT) trial,25 with 2,308 patients undergoing an intravascular angiographic procedure randomized to acetylcysteine vs placebo, and the previously mentioned PRESERVE trial.24 Both trials showed no difference in rates of AKI between the acetylcysteine and placebo groups.
Statins have been postulated to reduce the risk of CI-AKI because of their pleiotropic anti-inflammatory and antioxidant effects, which help stabilize plaque. There have been many conflicting studies, with recent meta-analyses suggesting a possible benefit in patients undergoing coronary angiography.10 Whether this benefit is due to prevention of CI-AKI or atheroembolic kidney disease is not clear. Most patients who undergo coronary angiography ultimately receive high-dose statin therapy anyway, making this a moot point.
Other interventions, including vitamin C, high-flow oxygen, and ischemic preconditioning are promising but the evidence remains lacking.
In summary, volume expansion with isotonic saline appears to be the only intervention with a possible benefit in preventing CI-AKI. This is probably important in patients deemed to be at intermediate to high risk (Table 2). Acetylcysteine has no role as a prophylactic measure, and bicarbonate-based fluids do not appear to offer an added benefit beyond volume expansion. Other preventive measures include using low- or iso-osmolar contrast media with the lowest necessary total dose.
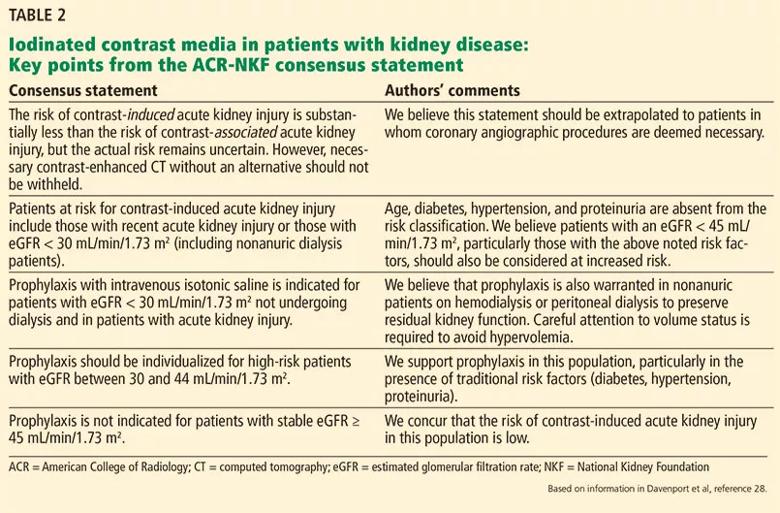
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/121405e0-95a9-49c8-acdd-4d40477b60ea/805x-Table-2_jpg)
We also advocate withholding nonsteroidal anti-inflammatory drugs, diuretics, angiotensin-converting enzyme inhibitors, and angiotensin II receptor blockers in high-risk patients, acknowledging that the data in that regard are insufficient.
Figure 1 shows our approach when patients with chronic kidney disease require iodinated contrast media.
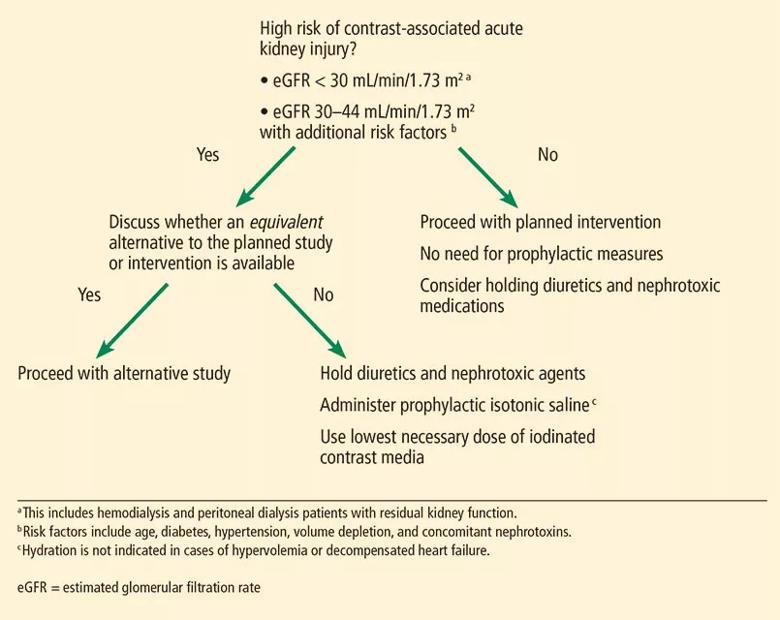
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b73198ba-a835-44e3-8a77-a82efbc7e2d6/805x-Figure-1_jpg)
Note that we generally include nonanuric patients undergoing hemodialysis or peritoneal dialysis in our high-risk category, and unless they are clinically hypervolemic, we recommend prophylaxis to preserve residual kidney function. A reanalysis of the Canada-USA (CANUSA) peritoneal dialysis study26 elegantly demonstrated that being able to produce as little as 250 mL of urine per day was associated with a 36% lower relative risk of death in peritoneal dialysis patients.
Although the data are less robust, this observation likely applies to hemodialysis patients as well, thus underscoring our recommendation for prophylaxis.27 We emphasize that the goal of hydration in this nonanuric dialysis population is not to make them hypervolemic, and as such, hydration should be forgone in overtly volume-overloaded patients.
The ideal hydration protocol for prevention remains uncertain, and various volume-expansion algorithms have been suggested using fixed or weight-adjusted regimens. Our practice is to give 1 to 1.5 mL per kg per hour starting one hour before and continuing for six hours after exposure to iodinated contrast media.
In response to the changing evidence, the American College of Radiology and the National Kidney Foundation released a joint consensus statement this year28 on the use of intravenous iodinated contrast media in patients with kidney disease. Key points are presented in Table 2.
Despite decades of research on iodinated contrast and kidney injury, many questions are yet to be answered. What is the exact mechanism of CI-AKI? What is its true incidence with intravenous vs arterial administration? What significance, if any, does CI-AKI carry?
In our aforementioned study,19 cases adjudicated to be CI-AKI carried no mortality risk, with an overall survival rate similar to that in patients who did not have AKI. Adjudication is key. We need clear definitions that capture CI-AKI clearly and distinctly from all the potential noise associated with other causes of postcontrast AKI.
The concept of “renalism” has not only led to fewer angiographic procedures being performed in the chronic kidney disease population,13 it probably also underlies the reason why patients with advanced CKD were less well represented in the observational cohorts described above. Studies need to target this high-risk cohort to better delineate the risks and better establish the utility, or futility, of the currently practiced prophylactic measures. Additional work is clearly needed.
Please note: This is an abridged version of an article originally published in the Cleveland Clinic Journal of Medicine. This is the first article in a two-part series; the article in its entirety, including a complete list of references, can be found here.
Advertisement

Pediatric urologists lead quality improvement initiative, author systemwide guideline

Fixed-dose single-pill combinations and future therapies

Reproductive urologists publish a contemporary review to guide practice

Two recent cases show favorable pain and cosmesis outcomes

Meta-analysis assesses outcomes in adolescent age vs. mid-adulthood

Proteinuria reduction remains the most important treatment target.

IgA nephropathy is a relatively common autoimmune glomerular disease that can be diagnosed only by biopsy

Oncologic and functional outcomes are promising, but selection is key