5 biggest changes according to Cleveland Clinic experts

The 2025 American College of Cardiology and American Heart Association guideline for managing patients with acute coronary syndromes (ACS) has updated and combined the 2013 and 2014 guidelines on ST-elevation and non-ST-elevation conditions.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Combining recommendations into a single document makes sense because when patients present with chest pain, we don’t immediately know their diagnosis,” says Cleveland Clinic interventional cardiologist Jacqueline Tamis-Holland, MD, a member of the 2025 guideline writing committee. “The initial evaluation to diagnose the presenting condition and the medical therapies we give to patients are often the same, regardless of whether or not there is ST elevation on the ECG. There is a similar evidence base for using medications, including statins, anticoagulants and antiplatelets.”
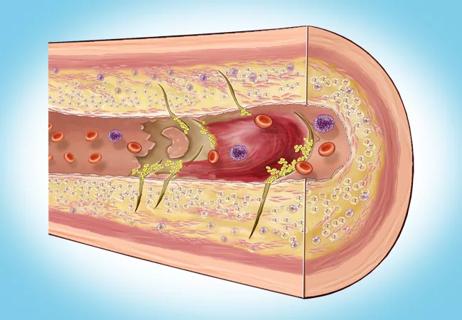
While ACS encompasses unstable angina, ST-elevation myocardial infarction (STEMI) and non-ST-elevation myocardial infarction (NSTEMI), the new guideline focuses solely on type 1 myocardial infarction (MI) resulting from presumed plaque rupture. The guideline does not address the management of other types of MI, such as those due to spontaneous coronary artery dissection, coronary embolism or coronary vasospasm, mostly due to a dearth of evidence-based management approaches, notes Dr. Tamis-Holland.
“Rigorous randomized clinical trials, in which we test new management strategies and identify proven treatments, give us the confidence to publish guidelines like this,” says Cleveland Clinic cardiologist Venu Menon, MD, another member of the guideline writing committee. “It is heartening for cardiologists to know that the recommended treatments for patients are predominantly based on proven evidence rather than individual opinion.”
Advertisement
Since the 2013 and 2014 guidelines were published, the medical management of ACS has been further refined, with new evidence supporting the completeness and timing of revascularization in the ACS setting. The 2025 guideline, published in both the Journal of the American College of Cardiology and Circulation, summarizes current care recommendations in a list of “Top Take-Home Messages.” Below, Drs. Menon and Tamis-Holland share what they view as the biggest changes for cardiologists in the new guideline.
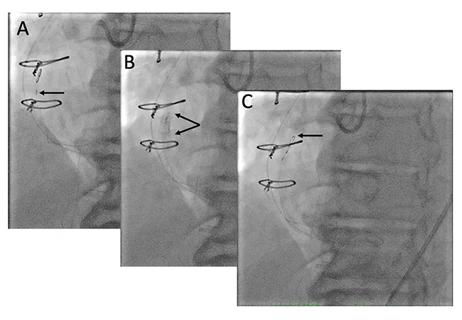
1. Use intracoronary imaging to guide percutaneous coronary intervention (PCI).
This recommendation was not included in prior STEMI and NSTEMI guidelines because intracoronary imaging to guide PCI was infrequently used a decade ago. It was included in the 2021 Guideline for Coronary Artery Revascularization as a class 2a (moderate) recommendation but has been elevated to a class 1 (strong) recommendation in the 2025 guideline.
“This upgrade in the class of recommendation for intracoronary imaging was based on newer evidence demonstrating that imaging during a PCI improves the outcomes of patients with complex disease,” Dr. Tamis-Holland says. “Imaging with intravascular ultrasound or optical coherence tomography can help ensure you use the right sized stent, identify situations in which there is underexpansion of the stent or dissections at the stent edges, and avert other complications. Studies have shown that when intracoronary imaging is used, patients are less likely to have restenosis or recurrent ACS, and they have better survival. Intracoronary imaging during PCI is commonplace at Cleveland Clinic, but all interventional cardiologists should be aware of its benefits and incorporate it into their routine practice.”
Advertisement
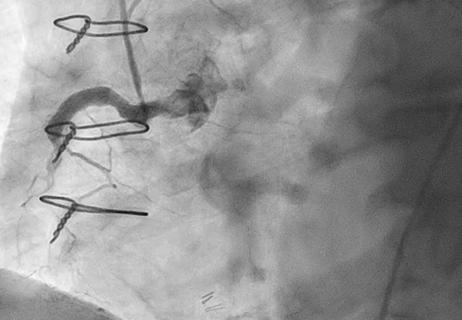
2. Perform complete revascularization for most patients with multivessel ACS.
The 2025 guideline strongly recommends (class 1) treating severely stenotic nonculprit arteries in addition to culprit arteries in patients with multivessel ACS.
Although the 2021 revascularization guideline also gave this a class 1 recommendation, it suggested performing complete revascularization in a staged procedure. Based on recent clinical trials, the 2025 guideline recommends that, when appropriate, PCI of severe lesions in nonculprit vessels now can be done either at the same time as the index procedure or later.
“The body of data over the past five-to-eight years is compelling and strongly supports consideration of complete revascularization in patients with ACS, whether STEMI or NSTEMI,” Dr. Menon says. “The only exception is for patients with ACS complicated by cardiogenic shock. The CULPRIT-SHOCK trial indicated that routinely performing PCI on noninfarct arteries in these hemodynamically unstable patients was associated with harm.”
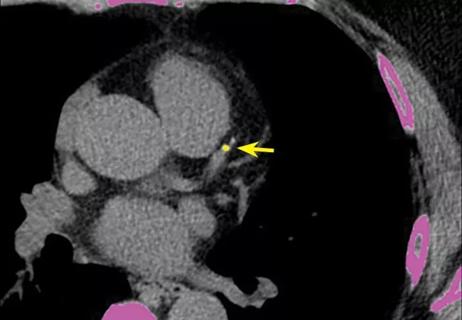
3. Consider mechanical circulatory support for patients with cardiogenic shock.
Microaxial flow pumps, which have become more prevalent in the past decade, now have a class 2a recommendation for use in patients with cardiogenic shock complicating acute myocardial infarction. The routine use of intra-aortic balloon pump or extracorporeal membrane oxygenation to provide temporary mechanical circulatory support in shock patients is not recommended (class 3).
“Cardiogenic shock is associated with a mortality rate of 45%-50% even with optimal revascularization of the infarct-related artery,” Dr. Menon says. “There had been little to no improvement in cardiogenic shock outcomes since the turn of the century, when the SHOCK trial first established the mortality benefit with emergency revascularization. However, in 2024, the DanGer Shock trial reported that using a temporary mechanical support device in the setting of acute MI and cardiogenic shock is associated with lower mortality.”
Advertisement
While data show that using mechanical support saves lives, it also is associated with significant complications (e.g., vascular injury, renal failure requiring renal replacement therapy).
“We haven’t yet synthesized the benefits versus the observed risks in the DanGer trial. That’s why using microaxial flow pumps has a class 2a recommendation in the 2025 guideline,” Dr. Menon says. “However, I’m encouraged by its presence in the guideline for the first time. We finally have a proven intervention that improves survival in these subjects.”
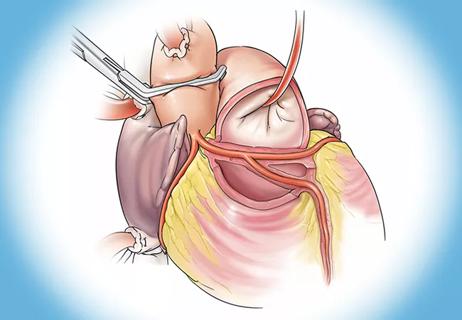
Also moderately recommended (class 2a) is using mechanical circulatory support as a bridge to surgery in patients with mechanical complications of shock, adds Dr. Tamis-Holland.
“This is a totally new recommendation,” she says. “We know that performing emergency surgery on patients with mechanical complications can be problematic because the cardiac tissue is often necrotic, making it difficult for the surgeon to provide adequate sutures. It takes time for the tissue to become fibrotic, so that the surgeon can have a more secure suture line. The use of mechanical circulatory support in these patients can help stabilize hemodynamics, improve end organ injury, promote tissue healing and enable postponement of definitive surgical intervention downstream.”
4. Prescribe dual antiplatelet therapy for only one month in patients with bleeding risk.
The recommendations for dual antiplatelet therapy (DAPT) are similar to the 2021 revascularization guideline, but now with additional strategies to consider for patients with high risk of bleeding or for reducing bleeding risk after treatment for MI. DAPT (aspirin and an oral P2Y12 inhibitor) for 12 months after ACS is routine. A new class 1 recommendation advises using DAPT for only one month followed by ticagrelor monotherapy to reduce the risk of bleeding.
Advertisement
The guidelines further emphasize the use of the more potent P2Y12 agents (i.e., ticagrelor, prasugrel) as first-line therapy.
“Clopidogrel should be reserved for patients who can’t tolerate or don’t have access to ticagrelor or prasugrel,” Dr. Tamis-Holland says. “We used to group the P2Y12 agents into one category with a slight preference for the more potent agents. However, ongoing evidence indicates that ticagrelor is preferred as a more effective and equally safe medication in most cases.”
5. Transfer patients to centers of excellence.
The 2025 guideline strongly recommends (class 1) transferring patients with cardiogenic shock to a medical center with expertise in managing them.
“Being at a center with a multidisciplinary heart team is the most important factor in ensuring the best outcomes for this vulnerable patient population,” Dr. Menon says.
Adds Dr. Tamis-Holland, “At Cleveland Clinic, we have been advocating this approach for many years. Any medical center (even outside our system) can request a consultation with the physicians and surgeons on our Shock Team. We are always happy to collaborate.”
While many of these new recommendations already are commonplace at Cleveland Clinic, Drs. Menon and Tamis-Holland are enthusiastic about having them recorded and accessible in a single document.
“The American College of Cardiology and the American Heart Association have committed to more frequent updates going forward, whenever new evidence becomes available,” Dr. Menon notes. “Over the next few years, we can expect to see regular modifications to make this a living document that best reflects optimal evidence-guided practice.”
Advertisement
While procedural success rates lag overall, they shine for retrograde crossing
Lower success rates, more hospital MACE seen with poor-quality distal targets

Important additions to a novel surgical technique
Retrospective findings from an executive health program spur interest in broader studies
Growing awareness of impact leads to proliferation of procedures

A reliable and reproducible alternative to conventional reimplantation and coronary unroofing

Cleveland Clinic-pioneered repair technique restores a 61-year-old to energetic activity
Inflammation found more predictive of events than LDL-C in pooled analysis of RCTs