Randomized controlled study undercuts unsubstantiated ‘heart health’ claims

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/7d1a432d-7bd7-4920-af62-ff1a4056f87d/22-HVI-3276958-supplement-pills_650x450-jpg)
pill tablets of various colors
Despite marketing claims, none of six dietary supplements commonly used for lipid lowering significantly reduced LDL cholesterol (LDL-C) versus placebo in adults with elevated atherosclerotic risk, finds the Supplements, Placebo or Rosuvastatin Study (SPORT). The results contrasted with a significant LDL-C reduction achieved with low-dose statin therapy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Findings of this Cleveland Clinic study were presented Nov. 6 in a late-breaking science session at the American Heart Association (AHA) Scientific Sessions and simultaneously published online in the Journal of the American College of Cardiology.
“Dietary supplements are widely used by people with indications for lipid-lowering therapy despite an absence of evidence for effectiveness in lowering LDL-C, especially relative to statin therapy,” says Cleveland Clinic cardiologist Luke Laffin, MD, who presented the study at the AHA meeting. “Few well-controlled trials have investigated supplements’ effects for this purpose, so we initiated this randomized, placebo- and statin-controlled trial to help fill the evidence gap.”
Marketing of dietary supplements is regulated under the Dietary Supplement Health and Education Act of 1994 and overseen by the U.S. Federal Trade Commission rather than the Food and Drug Administration. Consequently, supplements do not need to meet the standards for safety and efficacy required for marketing of pharmaceuticals.
This has enabled the marketing of numerous dietary supplements as natural alternatives to pharmaceuticals for promoting “cholesterol health,” “heart health” and similar claims. As a result, supplements marketed in this way account for a share of the nearly $50 billion spent annually on dietary supplements in the U.S. Consumer studies have shown that supplements are commonly used by patients for dyslipidemia in lieu of statins, with many U.S. consumers perceiving supplements as safer than and just as effective as statins.
Advertisement
“This represents a major public health concern,” says the study’s senior author, Steven Nissen, MD, Chief Academic Officer of Cleveland Clinic’s Miller Family Heart, Vascular & Thoracic Institute.
The SPORT trial was designed as a single-center, prospective, randomized, single-blind study of 199 adults with an LDL-C level of 70-189 mg/dL and an elevated 10-year risk of atherosclerotic cardiovascular disease (ASCVD) but no history of ASCVD. Participants were assigned equally to 28 days of treatment with one of the following (commercially available preparations were used for all supplements):
The primary endpoint was the percentage change in LDL-C; secondary endpoints included percentage changes in high-sensitivity C-reactive protein (hsCRP), high-density lipoprotein cholesterol (HDL-C), total cholesterol and serum triglycerides, as well as percentage changes in lipid and inflammatory biomarkers of each supplement relative to placebo.
Participants’ mean age was 64.4 years; 59% were women and 89% were of white race and non-Hispanic ethnicity. Mean baseline LDL-C was 128.2 (± 23.4) mg/dL. Overall, 190 participants completed follow-up lab testing and were included in the analysis.
While rosuvastatin significantly lowered LDL-C compared with placebo (35.2% relative reduction [95% CI, 29.5% to 41.3%], P < 0.001), none of the supplements did, and the garlic supplement was associated with a significant LDL-C increase versus placebo.
Advertisement
For secondary endpoints, patients receiving rosuvastatin showed a significantly greater percentage reduction from baseline in total cholesterol and in serum triglycerides compared with placebo and all supplements. No difference in HDL-C effects were observed between rosuvastatin and all comparators except for plant sterols, which significantly reduced HDL-C relative to rosuvastatin. No significant differences were observed between the groups in effect on hsCRP.
Adverse event rates were minimal and comparable across all study groups.
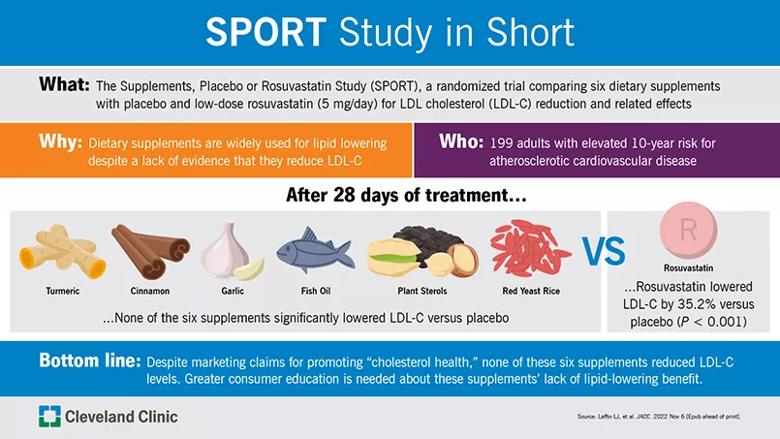
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c61cfbaa-6ac9-44d1-a5cf-e1e6d24fd54b/22-HVI-3365135-SPORT-trial-CQD-805_jpg)
“Despite a lack of evidence, use of dietary supplements has risen exponentially in the past three decades, including for dyslipidemia,” says Dr. Laffin. “Our finding of no significant reduction in LDL-C relative to placebo with any of these six supplements runs counter to the ‘cholesterol health’ claims made by supplement manufacturers.”
This discordance is underscored, he adds, by the supplements’ additional failure to demonstrate any significant effect on other lipid or inflammatory biomarkers compared with placebo, again in contrast to the positive results observed with rosuvastatin 5 mg/day.
In their study report, the authors write that widespread patient preference for alternatives to statins is likely multifactorial and partly due to beliefs about hepatotoxicity, muscle symptoms and neurological side effects reported with statin use. They note that such concerns are inappropriately intensified by “an abundance of statin misinformation” against a backdrop of limited government regulation of supplements and their marketers’ claims. The result, they write, is “an environment that deters the U.S. population from taking well-regulated, inexpensive, safe, and potentially life-saving [statin] medications with decades of supporting evidence.”
Advertisement
The lack of robust regulation of dietary supplements has also led to frequent reports of product contamination and insufficient awareness of potentially dangerous interactions that supplements may have with other medications patients are taking.
“It’s not just that dietary supplements may be ineffective; they sometimes can be harmful,” says Dr. Nissen. That’s a notion supported by this study’s finding of a statistically significant increase in LDL-C levels with the garlic supplement, which aligns with some previously published studies.
“Our findings call for greater patient education about the lack of benefit of dietary supplements on important cardiovascular risk factors,” Dr. Laffin notes.
“The tens of billions of dollars spent on unsupported dietary supplements each year is wasted, when it could be spent on productive healthcare,” Dr. Nissen adds. “More must be done to change that.”
Advertisement
Advertisement
Phase 3 TANDEM study may help pave way to first approval of a CETP inhibitor
Reassurance from the lipid outcomes trial with the highest percentage female enrollment to date
Tech-assisted self-selection concurred with clinician-assessed eligibility in >90% of cases
Robust reductions in cardiac events seen in high-risk patients without prior events
Findings bolster the oral drug as an option for primary and secondary prevention
Effect on gut microbiome emerges as another benefit of statin therapy
First-in-human phase 1 trial induced loss of function in gene that codes for ANGPTL3
A reliable and reproducible alternative to conventional reimplantation and coronary unroofing