Multidisciplinary approach can uncover unsuspected diagnoses

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ba71359c-a56e-498e-9400-3e2a14d537ff/650x450-Interstitial-Lung-Disease-Outcomes_jpg)
650×450-Interstitial-Lung-Disease-Outcomes
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
There are between several dozen and over 200 interstitial lung diseases (ILDs), depending on how they are classified. With the release of the INBUILD trial, the ascendant concept of a progressive fibrotic phenotype has been interpreted to imply that diagnostic precision is no longer relevant.
On the contrary, within Cleveland Clinic’s ILD team, we believe that a careful and specific diagnosis remains central to best outcomes for ILD patients. Knowledgeable and circumspect diagnosis is the cornerstone of ILD practice. We have routinely observed that a multidisciplinary approach can uncover unsuspected diagnoses, and many times this precision makes a difference in management strategy and effectiveness of treatment.
Figure 1 depicts the final diagnostic outcome of all 1,767 patients seen in 2019 by Cleveland Clinic’s ILD team and who had more than one visit to our center, even if the first visit was prior to 2019. Forty-five percent of patients (498 of 1,115) with a suspected referring diagnosis were found to carry an alternative or unclassifiable diagnosis after a comprehensive assessment; 80% of patients referred without a defined diagnosis had a specific diagnosis rendered by the end of 2019.
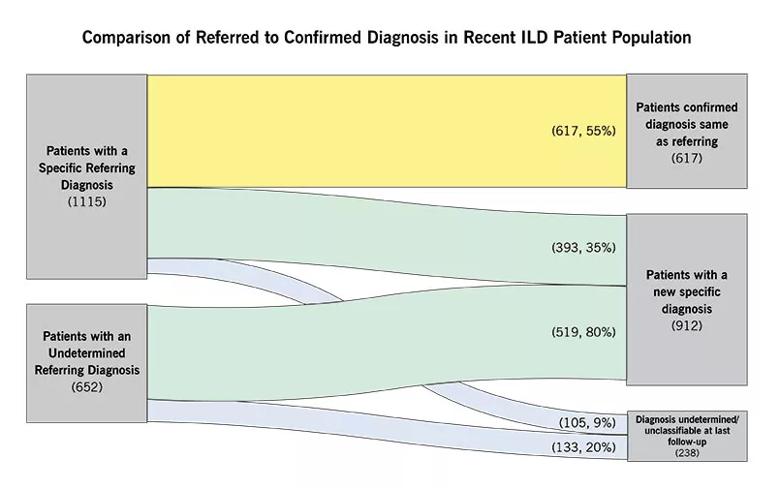
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/83329b47-5745-43eb-a4f8-93cb3213e737/805x-Chart-1_jpg)
Figure 1
Considering the deadliest ILD, idiopathic pulmonary fibrosis (IPF), nearly 30% of patients referred with the diagnosis of IPF were found to have an alternate explanation (81 of 279 referrals, Figure 2). This is significant because many other diagnoses present more effective treatment options and carry a better prognosis than IPF.
Advertisement
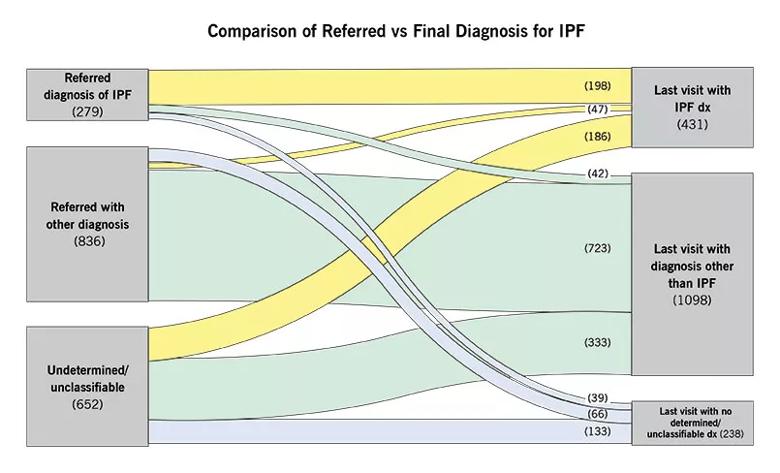
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/229c2f3e-ed05-4718-a780-e04c2a5cae67/805x-Inset-2_jpg)
Figure 2
Early referral to a tertiary center has been shown to improve outcomes for patients with IPF, an observation that is likely to be due at least in part to diagnostic precision.
Defining a specific diagnosis may be most important in cases where rare or unrecognized causes for ILD are present. For example, identification of a triggering etiology for hypersensitivity pneumonitis is associated with better outcomes, likely because exposure can thereby be avoided. The use of immunosuppressive therapy, primarily mycophenolate, was associated with better preservation of lung function in the SENSCIS trial when compared with nintedanib monotherapy in scleroderma lung disease. This observation underscores the relevance of identifying underlying connective tissue disease in ILD patients.
Prior studies have shown that academic teams are less likely than community pulmonologists to confer a diagnosis of IPF, highlighting the value of the broader differential diagnoses entertained in more experienced centers. The combination of subspecialized expertise, a full range of diagnostic modalities and higher patient volume probably contributes to diagnostic acumen.
A key feature of careful diagnosis is the multidisciplinary discussion (MDD). Besides diagnosis of the most challenging cases, MDD is used in our center prior to subjecting patients to any invasive procedures, and for discussion of difficult aspects of management. The emergence of new technologies, including cryobiopsy and molecular classifiers, supports an even greater role for MDD prior to invasive procedures. In our center, proposed invasive diagnostic testing is withheld as likely noncontributory in 44% of patients reviewed prior to such procedures.
Advertisement
Increasingly, unclassifiable ILD has been recognized as a significant fraction of all ILD. The question of whether conferring a label of unclassifiable requires a biopsy, and what type of biopsy, remains unsettled. In our center, we classify patients as “undetermined” when the diagnostic testing is incomplete (e.g., unfinished, or when any type of biopsy has not been obtained), reserving “unclassifiable” for only those patients who have completed all diagnostic steps including a biopsy. Combining these two categories, approximately 14% of our patients do not have a specific diagnosis, a proportion that is similar to that described elsewhere. It is recognized that radiographic and clinical features will be key determinants of therapies and prognoses in this subgroup.
Given the constraints of resource limitations, most patients with ILD seen at large centers like ours are not reviewed at the multidisciplinary conference. Data from large registries suggest that only approximately one-quarter of IPF patients are reviewed at MDDs.
Although there are relatively few data that suggest improved outcomes using MDD, there is well-substantiated evidence demonstrating that MDD improves diagnostic agreement. Certain diagnoses, such as hypersensitivity pneumonitis, exhibit poor diagnostic agreement between MDDs at different institutions. Nonetheless, the MDD process has been deemed to be a central tenet of modern ILD care, and it is a weekly component of our ILD practice.
Molecular techniques using lung tissue, blood and other biosamples, in combination with deep learning algorithms for radiographic interpretation, will revolutionize the classification and diagnosis of ILDs. Endotypes derived from molecular studies will inform management and lead to novel biologic insights. Until that time, rigorous efforts to provide accurate diagnoses will continue to be crucial for management of ILD.
Advertisement
Dr. Culver is Director of the Interstitial Lung Disease Program in Cleveland Clinic’s Respiratory Institute.
Advertisement
Advertisement
Takeaways from the most recent annual meeting centered around clinical advances, AI integration and professional development
Recent breakthroughs have brought attention to a previously overlooked condition
A review of treatment options for patients who may not qualify for surgery
Looking at the real-world impact and the future pipeline of targeted therapies
The progressive training program aims to help clinicians improve patient care
New breakthroughs are shaping the future of COPD management and offering hope for challenging cases
Exploring the impact of chronic cough from daily life to innovative medical solutions
How Cleveland Clinic transformed a single ultrasound machine into a cutting-edge, hospital-wide POCUS program