Treatments can be effective, but timely diagnosis is key
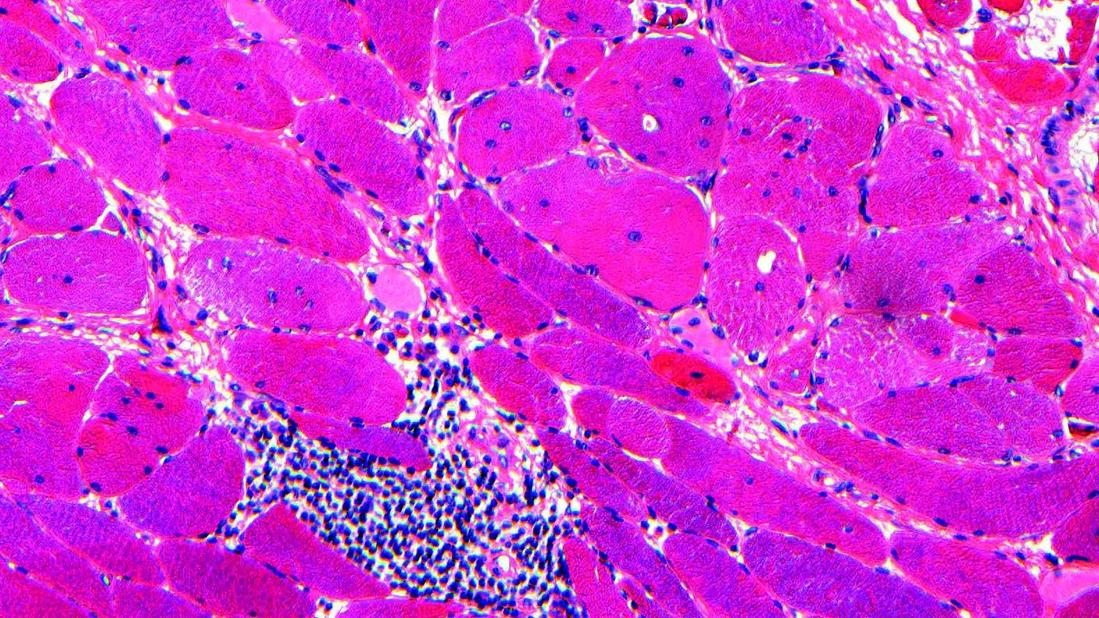
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b10fcf9c-7e90-456b-b132-5511bf1bf547/muscle-biopsy-cells-indicating-myositis)
Myositis
Interstitial lung disease is a leading cause of morbidity and mortality for patients with inflammatory autoimmune diseases. Immune-mediated myositis (IIM) is an autoimmune disease that can affect multiple organs simultaneously, most commonly the muscle, skin and lungs.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The diagnosis can be challenging in patients who present with isolated lung disease in the absence of other organ involvement.
Providers may not suspect an inflammatory disease, like myositis, when a patient presents with breathing problems, notes Cleveland Clinic pulmonologist Sameep Sehgal, MD. “The biggest challenge is recognizing that you may have an autoimmune disease that is only manifesting as inflammation in the lungs,” he says. “It doesn’t necessarily have to meet all the usual things we think about with autoimmune disease, like joint problems, skin rash or muscle pain.”
Appropriate treatment can be lifesaving, so making an accurate and timely diagnosis is key, he adds.
Interstitial lung disease is the most common lung disease seen in IIM patients. It affects about 40-50% of all IIM patients, with severity ranging from mild to life-threatening disease. The two subtypes of IIM, it is even more common with a prevalence of around 90% of patients in those with anti-synthetase syndrome or anti-MDA-5 antibody dermatomyositis. In about 20% of IIM patients, lung disease may be the only manifestation.
Many patients initially present to a rheumatologist with muscle pain, joint pain and inflammation, and they are subsequently also found to have lung problems, Dr. Sehgal says. In other cases, the patient may first be seen by a pulmonologist.
“Very often they present with shortness of breath, coughing and low oxygen numbers, and we end up finding that they have inflammation in the lungs or ILD,” he says. “Then, we go down the pathway of figuring out what’s causing it, and in that process, we find out that they also have myositis, or immune-mediated myositis.” In the most severe cases, patients may present to the ICU in respiratory failure.
Advertisement
Diagnosing typically starts with a detailed history, physician examination, breathing tests and imaging, such as a CT scan of the lungs. Blood tests to measure markers of inflammation (ESR, CRP), muscle damage (CPK, aldolase) and presence of auto-antibodies. Additional tests such as muscle imaging, EMG or biopsies (lung, muscle or skin) might be needed.
A diagnosis of myositis-related lung disease should be based on the combination of the patient’s clinical profile, chest imaging and results of auto-antibodies stresses Dr. Sehgal.
“There is not one specific test that we rely on for the diagnosis,” he says. “It’s a combination of several different things. You may have a negative antibody test, but in the right clinical setting, the diagnosis could be myositis lung disease. On the other hand, you may have a positive antibody test, but if nothing else fits, it’s unlikely to be that. So, it’s important to look at all the information.”
Dr. Sehgal says the complexity of diagnosis and treatment is one reason multidisciplinary care is key. Pulmonology, rheumatology, neurology, dermatology and other specialists may be involved in helping manage the disease.
Cleveland Clinic has established a rheumatic lung disease program to facilitate collaboration between pulmonologists and rheumatologists. Specialists within the program either share cases or consult on patients being treated separately.
Treatment can include a combination of steroids, immunosuppression, antifibrotic medications, pulmonary rehabilitation or lung transplantation. The intensity of treatment depends on the disease severity and rate of progression. In patients with rapidly progressive lung disease, early, combination immune suppression is essential and in those with more chronic ILD and incremental approach to treatment can be taken.
Advertisement
“If the patient has primary lung involvement, the pulmonologists take over treatment and decide how aggressive we need to be,” Dr. Sehgal explains. “If the main organ or the muscle or skin is involved, then the rheumatologist would take the lead on patient care. There’s a lot of discussion and collaboration, and things often change over time.”
It’s important for providers to know that treatment is available and can be effective. “Myositis lung disease often responds to treatment with a five-year survival rate of 80% to 90% in those with chronic ILD,” he says. “However, in patients with rapidly progressive ILD or those with the anti-MDA5 DM subtype, the disease can progress rapidly and be refractory to treatment.” Recognizing it, making the right diagnosis and treating it appropriately can have a real impact on how the patient does.
Advertisement
Advertisement
A review of treatment options for patients who may not qualify for surgery
Rising rates in young miners illustrate the need for consistent prevention messaging from employers and clinicians
Multidisciplinary focus on an often underdiagnosed and ineffectively treated pulmonary disease
Management and diagnostic insights from an infectious disease specialist and a pulmonary specialist
A Cleveland Clinic pulmonologist highlights several factors to be aware of when treating patients
Patient experience improves with a multidisciplinary approach
A mindset shift has changed the way pulmonologists both treat and define PFF
Collaborative patient care, advanced imaging techniques support safer immunotherapy management