May allow greater independence and quality of life
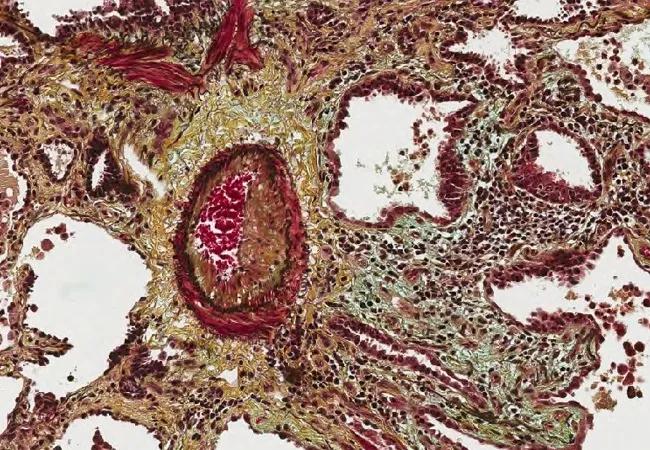
Pulmonary hypertension has been reported in up to 86% of patients with interstitial lung disease and is associated with reduced exercise capacity, greater need for supplemental oxygen, decreased quality of life and earlier death.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Despite the prevalence and poor clinical course of pulmonary hypertension due to interstitial lung disease (PH-ILD: WHO Group 3), no approved therapies were available to treat these patients. Then in April 2021, the results of a randomized, placebo-controlled study called INCREASE led the U.S. Food and Drug Administration to green light the use of inhaled treprostinil (Tyvaso®) for the treatment of patients with Group 3 PH-ILD.
Cleveland Clinic pulmonologists, who have been using inhaled treprostinil for years and were aware of its potential benefits, welcomed the news.
“Patients in Group 3 have a terrible prognosis, so it is a relief to have something that might be moving the needle,” says Kristin Highland, MD, Research Director of Cleveland Clinic’s Respiratory Institute and a pulmonologist who treats both PH and ILD. “It may not extend their life, but it will allow them greater independence and a better quality of life.”
Treprostinil is a stable analogue of prostacyclin that promotes direct vasodilation of pulmonary and systemic arterial vascular beds and inhibits platelet aggregation.
An inhaled formulation of treprostinil was previously shown to improve exercise capacity after 12 weeks of therapy in patients with WHO Group 1 pulmonary arterial hypertension (PAH). It was approved for this indication in 2009.
Pilot studies suggested that inhaled treprostinil improved hemodynamics and functional capacity in patients with Group 3 PH-ILD. The INCREASE study was designed to evaluate the safety and efficacy of inhaled treprostinil in these patients.
Advertisement
INCREASE randomized 366 patients to inhaled treprostinil or placebo. Participants randomized to the study drug experienced a significant improvement in exercise capacity as assessed by 6-minute walk distance. Compared with placebo, inhaled trepostinil also was associated with lower risk of clinical worsening, greater reduction in N-terminal pro b-type natriuretic peptide (NT-proBNP) and fewer exacerbations of underlying lung disease during the 16-week treatment period.
Concern that inhaled drug could worsen ILD led the researchers to monitor the patients with pulmonary function tests. To their surprise, the study participants on treprostinil showed improvement in forced vital capacity.
“This is really exciting and has resulted in new hypothesis that the drug may not only induce vasodilation, but may also have antifibrotic properties. This would be earth shattering,” says Dr. Highland.
Cleveland Clinic pulmonologists will participate in a study designed to evaluate the effect of inhaled treprostinil on fibrosis. Additionally, they are awaiting the results of a study of inhaled treprostinil in COPD.
Without an approved therapy for Group 3 PH-ILD, pulmonologists have treated patients with systemic pulmonary vasodilators approved only for the treatment of Group 1 PAH. However, there was concern that such agents could worsen ventilation-perfusion matching.
“The risk was that giving an oral, intravenous or subcutaneous drug to patients with ILD might worsen oxygenation,” Dr. Highland explains.
Advertisement
On the other hand, it was theorized that an inhaled drug would redirect blood flow to the healthiest lung units, thereby preserving oxygenation.
“Indeed, in the current trial, we saw no evidence of worsening oxygenation, which alleviated our concerns about ventilation-perfusion mismatching,” she says. “Our experience had confirmed this, and it was reassuring to have data supporting this clinical behavior.”
The optimal care of patients with Group 3 PH-ILD is best accomplished by close collaboration between experts in ILD and PH.
“This is not a drug most general pulmonologists will prescribe,” says Dr. Highland. “It’s better to refer your patients to a PH expert, or at least request one consultation.”
Dr. Highland and her colleagues who treat PH have developed a protocol for screening patients with ILD who might have PH and, therefore, benefit from inhaled treprostinil. The protocol helps determine which patients with PH should receive the drug.
“This is a very expensive drug, so if a patient is headed toward hospice, prescribing the drug will not be appropriate,” she says. “Now that inhaled treprostinil is FDA-approved, however, it will be easier to get insurance coverage for it, and that’s a huge relief.”
Advertisement
Advertisement

Takeaways from the most recent annual meeting centered around clinical advances, AI integration and professional development

Recent breakthroughs have brought attention to a previously overlooked condition

A review of treatment options for patients who may not qualify for surgery

Looking at the real-world impact and the future pipeline of targeted therapies

The progressive training program aims to help clinicians improve patient care

New breakthroughs are shaping the future of COPD management and offering hope for challenging cases

Exploring the impact of chronic cough from daily life to innovative medical solutions

How Cleveland Clinic transformed a single ultrasound machine into a cutting-edge, hospital-wide POCUS program