Why experts advise against it for breast, skin and gynecologic cancers
Traditional brachytherapy involves placing a radioactive source inside or on the surface of a patient’s body to more directly target a cancer or at-risk site. Used alone or in combination with external beam radiation therapy, it is standard of care for several types of malignancies.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Traditional brachytherapy techniques are categorized as low dose rate, pulsed or high dose rate, based on how the radiation sources decay. They can be left in the body permanently, such as with radioactive seeds to treat prostate cancer, or temporarily, such as with implants or applicators used to treat gynecologic or breast cancers.
While it is effective, isotope-based brachytherapy comes with strict regulations and costs associated with managing radioactive sources. That’s partly why a new form of brachytherapy, electronic brachytherapy (EB), has gained prominence in the past 10 years.
EB uses electrically generated X-rays rather than radioactive isotopes. It is not regulated by the Nuclear Regulatory Commission, doesn’t require as much shielding (due to lower energies) and, as such, can be easy to administer.
“EB is intended to be an alternative form of brachytherapy,” says radiation oncologist Chirag Shah, MD. “However, how that radiation is generated and delivered is markedly different than traditional brachytherapy. Its dosing and clinical implications are still being studied.”
In 2018, the American Brachytherapy Society appointed a group of brachytherapy experts, including Dr. Shah, to establish guidelines for using EB. Based on a literature review and their clinical experience, the group published a consensus statement in Brachytherapy.
In the statement, the group revealed significant gaps in data about EB, even though it has been studied in:
Breast cancer. Using EB for partial breast irradiation showed good local control and acceptable toxicity in one study of nearly 1,000 women with early-stage breast cancer. Smaller studies indicated the same. However, few and only very small studies have tracked patients long-term (five years or longer).
Advertisement
Skin cancer. There are significant data supporting the use of brachytherapy for small skin cancers, but the use of EB, specifically, has not been studied long-term. Also, very little data compare EB with other radiation therapy or surgical techniques, and studies have focused mostly on older patients.
Gynecologic cancer. While it’s feasible to use EB to deliver radiation to the vaginal cuff (after removal of the cervix and uterus), only very small studies have evaluated its effectiveness. Larger studies of brachytherapy for gynecologic cancer have not included EB.
“We found that there weren’t a lot of data studying EB in a prospective, randomized way, as with traditional brachytherapy,” says Dr. Shah. “And we can’t extrapolate from other brachytherapy techniques to EB. It’s not certain you’ll always get the same dose delivered in the same way as traditional techniques, so we can’t be sure about clinical outcomes, toxicity and other factors.”
More data on EB from a larger number of patients, with longer follow-up, are needed.
Why is research in EB lacking? It could be because it’s not as widely used as traditional brachytherapy techniques.
Interest in EB may be greater in smaller centers not able to offer traditional brachytherapy due to regulatory and cost limitations, notes Dr. Shah — not in large brachytherapy programs that have other resources.
Until EB gains broader acceptance in the medical community and begins to be included in more long-term national trials, physicians can’t know how it could and should be used.
Advertisement
“EB could be a viable brachytherapy option, just not yet,” says Dr. Shah. “For now, our recommendation is not to use EB outside of clinical registries or trials.”
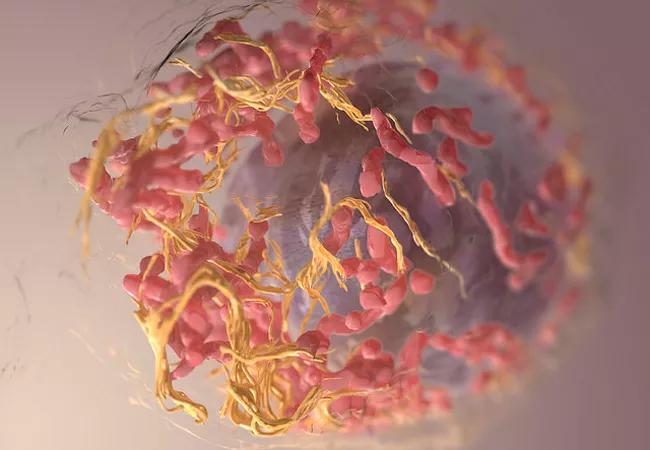
Feature image: 3D structure of a melanoma cell derived by ion abrasion scanning electron microscopy. Source: National Cancer Institute, created by Sriram Subramaniam
Advertisement
Advertisement

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists

Structured interventions enhance sleep, safety and caregiver resiliency in high-acuity units

Addressing rare disease and challenging treatment course in an active young patient