Intermediate-term results of REGROUP trial extend earlier findings
The safety of endoscopic vein harvesting for coronary bypass operations got a boost from intermediate-term results of the multicenter Randomized Endo-Vein Graft Prospective (REGROUP) trial.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Over median follow-up of 4.7 years, there was no significant difference in rates of major adverse cardiac events between coronary artery bypass graft (CABG) patients who underwent endoscopic vein harvesting versus open vein harvesting, according to a research letter by the REGROUP investigators published in JAMA Network Open on March 15.
The updated results follow similar findings through 2.7 years as reported by the REGROUP investigators two years ago (N Engl J Med. 2019;380:132-141) .
“Endoscopic vein harvesting was introduced in the 1990s with the aim of lowering rates of leg wound complications among patients undergoing CABG, but subsequent data suggested this harvesting method might be associated with elevated mortality relative to open vein harvesting,” says REGROUP co-investigator Faisal Bakaeen, MD, a cardiothoracic surgeon with Cleveland Clinic. “REGROUP was undertaken to explore this question in randomized controlled trial, and its findings continue to offer reassurance about the safety of endoscopic vein harvesting.”
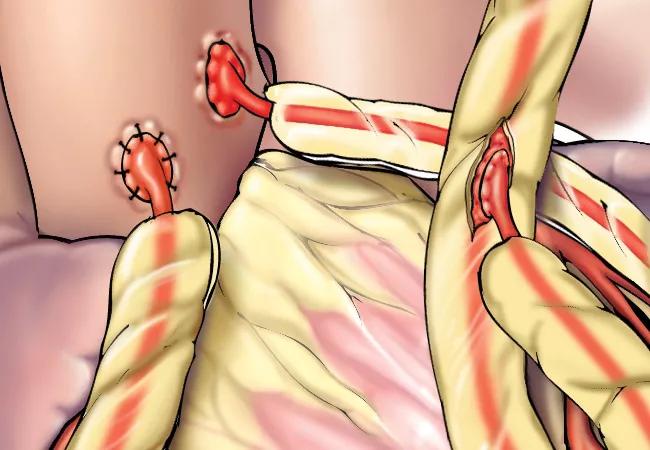
REGROUP researchers randomized patients undergoing CABG at 16 Department of Veterans Affairs (VA) medical centers to either endoscopic or open vein harvesting. Randomization took place among 1,150 patients from March 2014 through April 2017.
The primary outcome was the first occurrence of a major adverse cardiac event, i.e., a composite of all-cause mortality, nonfatal myocardial infarction (MI) or repeat revascularization.
Only expert endoscopic vein harvesters — defined as those who had performed over 100 such harvests with less than 5% conversion to open vein harvest — were eligible to perform the procedures. Eligible patients could undergo either elective or urgent CABG so long as the plan was to use at least one saphenous vein graft.
Advertisement
Patients were assessed at baseline, intra- and postoperatively, at discharge or 30 days after surgery, at six weeks, and then at every three months through at least one year. Thereafter patients were followed by merging VA and non-VA records and records from Medicare parts A and B.
The overall cohort was almost exclusively male (99.5%) and had a mean age at surgery of 66.4 years. The endoscopic and open harvesting groups were well matched by age, sex, smoking status, race/ethnicity, body mass index and comorbidities.
Median follow-up was 4.7 years (interquartile range, 3.8-5.5). Over this period the rate of a major adverse cardiac event was 21.9% in the endoscopic harvest group versus 23.5% in the open harvest group (hazard ratio = 0.92; 95% CI, 0.72-1.18; P = 0.52). Rates of each of the three components of the composite endpoint (death, MI, repeat revascularization) were numerically lower in the endoscopic group and statistically comparable between the groups.
The absence of statistical differences was maintained after adjusted multivariable Cox regression analysis.
While the REGROUP researchers note that their study was limited by the exclusive use of expert harvesters and a lack of imaging evaluation of graft patency, they conclude its intermediate-term results are nevertheless reassuring.
“Concern about potential long-term ischemic risk with endoscopic harvesting of saphenous vein grafts has resulted in variable uptake of this vein harvesting method,” says Dr. Bakaeen. “These findings about the enduring safety of this method in a head-to-head comparison with open vein harvesting support continued adoption of endoscopic harvesting when done by experienced experts.
Advertisement
“At the same time,” he continues, “it is important to put this in the context of expert consensus recommendations about using more arterial instead of venous conduits in appropriately selected patients in order to maximize the long-term benefits of CABG.”
The REGROUP investigators plan to continue follow-up through 10 years.
Advertisement
Advertisement

Scenarios where experience-based management nuance can matter most

Introducing Krishna Aragam, MD, head of new integrated clinical and research programs in cardiovascular genomics

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients