Residual AR related to severe preoperative AR increases risk of progression, need for reoperation
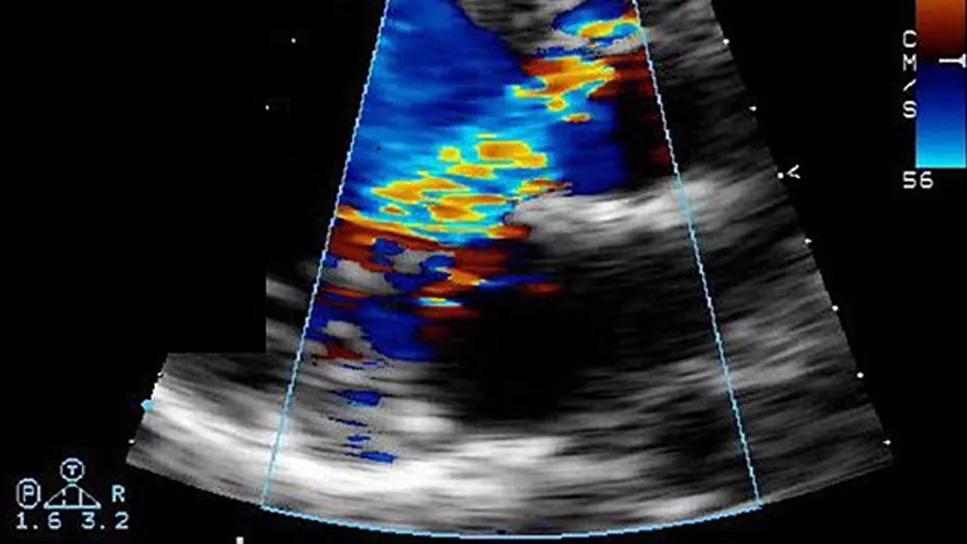
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/138040ff-076d-4b4c-a89c-c4c6bc7c6291/aortic-regurgitation)
echocardiogram showing severe aortic regurgitation
Predictors of residual aortic regurgitation (AR) after elective tricuspid aortic valve reimplantation include severe preoperative AR, smaller aortic root graft and concomitant cusp repair. And prevention of residual AR — an uncommon finding immediately following such operations — is important.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Those are two main conclusions of a retrospective analysis of more than 750 patients who underwent aortic valve reimplantation during elective repair of aortic root aneurysms at Cleveland Clinic over an 18-year period. Preoperative characteristics and postoperative outcomes of patients who had residual AR at hospital discharge were compared with those of patients without residual AR. The study was published in the Journal of Thoracic and Cardiovascular Surgery (2024;167[1]:101-111.e4).
“We noted that more severe preoperative AR was a predictor of residual AR and the need for leaflet repair,” says senior and corresponding study author Lars Svensson, MD, PhD, Chief, Cleveland Clinic Heart, Vascular & Thoracic Institute. “Although long-term survival rates were similar between those who did and did not have residual AR, risk of reoperation was higher if residual AR was present. It’s important to more closely follow patients found to have residual AR so that the need for reoperation can be recognized promptly.”
Aortic root replacement with valve-sparing aortic valve reimplantation has excellent outcomes, especially when performed electively in patients with aortic root aneurysm and a tricuspid aortic valve before AR is severe and the leaflets tear from the added stress of a dilated root. This makes successful reimplantation more difficult and requires leaflet repairs more often to save the valve. However, residual AR — noted either intraoperatively or before hospital discharge — may affect valve durability, and little is known about how it affects outcomes.
Advertisement
This single-center series was designed to characterize patients with residual AR after elective aortic valve reimplantation for aortic root aneurysm and compare baseline characteristics and postoperative and long-term outcomes between patients with and without residual AR.
The study population consisted of 756 patients (mean age, 50 years) who underwent elective tricuspid aortic valve reimplantation for aortic root aneurysm at Cleveland Clinic between 2002 and 2020. All patients underwent transthoracic echocardiography before hospital discharge. While uncommon, residual postoperative AR occurred in 65 of these patients (8.6%). The residual AR was predominantly classified as mild (n = 58), with rare moderate cases (n = 7). No patients had severe residual AR.
Patients were followed for a median of 3.3 years, with 25% followed for more than 7.5 years and 10% for more than 12 years.
The small subgroup of patients who had residual AR at discharge were more likely to have had severe AR preoperatively compared with those without residual AR at discharge (38% vs. 12%; P < .0001). Interestingly, having a connective tissue disorder did not predict residual AR.
Intraoperatively, those with residual AR were significantly more likely to have:
Advertisement
In-hospital outcomes were similar between the two groups, and no in-hospital deaths occurred. Long-term outcomes, assessed at 10 years, included the following differences between patients with residual AR at discharge compared to those without it:
Survival rates between the groups were similar at 10 years (97% among those with residual AR vs. 93% among those without; P = .43).
The risk of early reoperation was increased by the presence of residual AR; risk factors for late reoperation included concomitant coronary bypass, lower preoperative body mass index and lower preoperative ejection fraction.
Dr. Svensson points out that the rate of residual AR in this Cleveland Clinic series was less than 10%, which is lower than the rate of 25% to 29% reported in another large published series. Residual AR of greater than mild severity was exceedingly rare, occurring in less than 1% of all patients in the series. He notes that a certain measure of expertise is required to repair damaged leaflets in order to preserve a valve with associated tears and severe preoperative AR.
“Cleveland Clinic’s large surgical volume and extensive experience with concomitant valve repair likely are important reasons for these low rates,” Dr. Svensson says. “But other factors should also be noted.”
Specifically, he recommends the following.
Advertisement
“Although residual AR should be avoided if possible, its avoidance should not be the overarching goal when selecting surgical candidates or choosing reimplantation over replacement,” notes Dr. Svensson. “Causing a patient to go from severe to mild regurgitation should also be considered a successful outcome.”
“This is an important study that highlights the value of early and detailed evaluation of significant AR in the setting of a dilated aortic root,” adds cardiologist Milind Desai, MD, MBA, Medical Director of Cleveland Clinic’s Aorta Center, who was not involved in the study. “Such an evaluation would enable early referral to an experienced center for a valve-sparing root replacement, giving the patient the best chance of AR-free survival in the future.”
Advertisement
Advertisement
New Cleveland Clinic data challenge traditional size thresholds for surgical intervention
Study finds comparable midterm safety outcomes, suggesting anatomy and surgeon preference should drive choice
New review distills insights and best practices from a high-volume center
Blood test can identify patients who need more frequent monitoring or earlier surgery to prevent dissection or rupture
Recent Cleveland Clinic experience reveals hundreds of cases with anatomic constraints to FEVAR
Multicenter pivotal study may lead to first endovascular treatment for the ascending aorta
Large cohort study finds significant effect in men and nonsmokers
Impacts include major emphases on multidisciplinary teams, shared decision-making