But improvements didn’t correlate closely with physician-assigned NYHA class, study finds
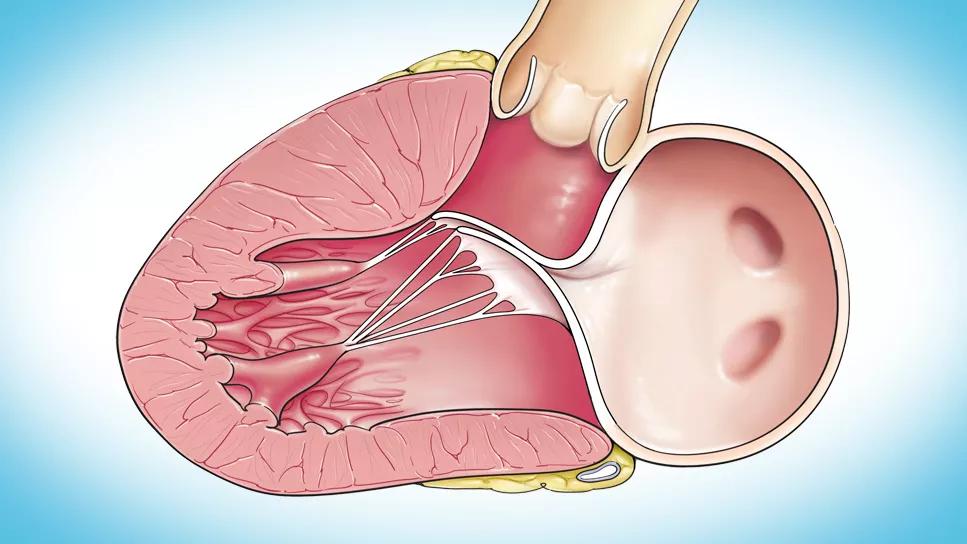
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d44767f5-7bbc-477a-b08c-2e6fbd24f727/systolic-anterior-motion-feature)
23-HVI-4317308_septal-myectomy_650x450
Patient-reported outcomes (PROs) are significantly improved after septal myectomy for obstructive hypertrophic cardiomyopathy (oHCM), but they do not necessarily correlate closely with physician-reported New York Heart Association (NYHA) class. So finds an analysis by Cleveland Clinic researchers of follow-up data from symptomatic patients in the SPIRIT-HCM study.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“At 12-month follow-up in symptomatic oHCM patients, septal myectomy significantly improved patient-reported outcomes, left ventricular outflow tract (LVOT) obstruction and functional capacity,” says senior author Milind Desai, MD, MBA, Director of Cleveland Clinic’s Hypertrophic Cardiomyopathy Center. “However, the results also underscore the discrepancy between what patients report about their quality of life, in terms of patient-reported outcome measures, and how physicians perceive their symptoms.”
The new analysis, published in Progress in Cardiovascular Diseases (2023;80:66-73), adds to a previous report of results from the single-center SPIRIT-HCM trial (JAMA Netw Open. 2022;5[4]:e227293), which showed that in patients with oHCM, septal myectomy significantly improves Kansas City Cardiomyopathy Questionnaire (KCCQ) scores for quality of life (QOL) as well as physical and health status.
The investigator-initiated, single-arm SPIRIT-HCM study prospectively enrolled 173 symptomatic adults aged 18 to 65 with oHCM who were undergoing surgical septal myectomy at Cleveland Clinic; all were in NYHA class II or III/IV at baseline. Three outcomes were assessed in the new analysis: the association between various PROs, their association with NYHA class and changes after septal myectomy.
Historically, observational studies of septal myectomy for HCM have used NYHA class to measure outcomes. “Quality-of-life assessment with patient-reported outcomes increasingly is being accepted as a more reliable outcome metric, and one better aligned with patient perception of physical and mental function,” Dr. Desai notes.
Advertisement
The PROs used to assess patients at baseline and 12 months post-procedure were KCCQ scores, the Patient-Reported Outcomes Measurement Information System (PROMIS), the Duke Activity Status Index (DASI) and the European QOL score (EQ-5D). None of those instruments were specifically designed to assess QOL in patients undergoing interventions for oHCM.
NYHA class, results of a 6-minute walk test (6MWT) and peak LVOT gradient also were recorded at baseline and 12 months.
At baseline, 35% to 49% of patients in NYHA class II had PRO scores worse than the cohort median, whereas 30% to 39% of patients in NYHA class III//IV had PRO scores better than median.
“This cohort had a median baseline KCCQ summary score that was worse than has previously been reported in oHCM studies, which suggests our patients were a sicker population and had substantially impaired quality of life,” observes study co-author Maran Thamilarasan, MD, staff cardiologist in Cleveland Clinic’s Section of Cardiovascular Imaging.
At 12 months after surgery, the authors found the following:
Notably, there was a highly statistically significant internal consistency among the various PROs, both at baseline and following myectomy. The magnitude of benefit of the procedure on the individual PROs also was very high.
Advertisement
In contrast, post-surgery improvements were more modest in physician-assessed NYHA class, with only 67% of patients assigned to class I at 12 months, and in peak LVOT gradient and 6MWT. Both at baseline and during follow-up, there was substanial overlap of PRO results within various NYHA classes.
“Our findings demonstrate that patients’ perceptions of their symptoms, physical and mental function, and quality of life cannot necessarily be ascertained from objective measures such as exercise stress testing,” says study co-author Nicholas Smedira, MD, MBA, Surgical Director of Cleveland Clinic’s Hypertrophic Cardiomyopathy Center. “This underscores the importance of directly assessing patient-reported outcomes.”
He adds that the study findings did not surprise him: “Post-myectomy, many patients send me cards and letters saying they cannot remember feeling so well, that they can run and hike and play with their children again without getting short of breath or lightheaded. It is truly life-changing for patients.”
The researchers noted that 6MWT results and PROMIS mental domain scores did not improve in a significant proportion of patients after myectomy. On follow-up, only 44% of patients increased their 6MWT result beyond 100 meters. Factors that the authors believe may be contributory ― and that they intend to investigate in future studies ― include diastolic dysfunction, overzealous beta blockade, obesity and deconditioning associated with long-term physical activity restriction prior to surgery.
Advertisement
Other areas for exploration include better defining the heterogeneity of the benefits of myectomy by examining which social, demographic, clinical and physiologic parameters are most strongly associated with improved status (or lack thereof) in patients with oHCM.
“In future trials, patient-reported outcomes, rather than NYHA class, should be emphasized as inclusion criteria and/or endpoints for judging success,” says Dr. Desai. “In addition, the patient-reported outcomes we assessed can be used to guide clinical management and make decisions about drug titration or recommendations for invasive therapies.”
Advertisement
Advertisement
Large single-center series demonstrates safety and efficacy for extending procedure
End-of-treatment VALOR-HCM analyses reassure on use in women, suggest disease-modifying potential
Cardiac imaging substudy is the latest paper originating from the VANISH trial
Vigilance for symptom emergence matters, a large 20-year analysis reveals
Phase 3 ODYSSEY-HCM trial of mavacamten leaves lingering questions about potential broader use
Our latest performance data in these areas plus HOCM and pericarditis
Tailored valve interventions prove effective for LVOTO without significant septal hypertrophy
5% of flagged ECGs in real-world study were from patients with previously undiagnosed HCM