Difficult to diagnose, treat
By Rula Hajj-Ali, MD, and W.H. Wilson Tang, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Eosinophilic granulomatosis with polyangiitis (EGPA) is considered a rare, orphan type of antineutrophilic cytoplasmic antibody (ANCA)- associated vasculitis. The disease is chronic with major morbidities involving vital organs including the heart, nervous system and kidneys. Asthma exacerbations remain a problematic manifestation that often do not respond to immunosuppressive treatment and thus require high doses of glucocorticoids.
I recently discussed the challenges and prognosis of this peculiar disease at the crossroads of primary systemic vasculitides and hypereosinophilic disorders at the Primary Vasculitides Presymposium hosted by Cleveland Clinic. I also asked my colleague Wilson Tang, MD, Director for Clinical Genomics and staff in the Heart and Vascular Institute, to discuss EGPA and the heart.
EGPA is an eosinophil-rich and necrotizing granulomatous inflammation often involving the respiratory tract. This necrotizing vasculitis predominantly affects small to medium vessels and is often associated with asthma and eosinophilia, with common findings of nasal polyps and granulomatous and nongranulomatous extravascular inflammation. Formerly called Churg-Strauss Syndrome, this multisystemic disease mostly affects patients between 40 and 60 years old, and its prevalence is 10.7 to 13 cases per million. Often, the diagnosis of EGPA is complex and requires collaboration from different disciplines including pulmonology, rheumatology, allergy and cardiology.
A major area of controversy in EGPA includes classification in the absence of proven vasculitis or, alternatively, in the presence of ANCAs or other vasculitis surrogate markers. Multiple studies have classified EGPA based on phenotype and presence or absence of ANCA, with a consensus of association of ANCA positivity with kidney and peripheral nervous system involvement and constitutional symptoms. ANCAs are present in about 40 percent of cases of the disease and are more frequent when glomerulonephritis is present. Limited expressions of EGPA confined to the upper or lower respiratory tract may occur and may pose a diagnostic challenge with other eosinophilic-associated diseases. ANCA alone may not be sufficient to diagnose vasculitis in EGPA patients. Further, it is clear that EGPA is a polygenic disease with different gene susceptibility in ANCA-positive and ANCA-negative patients.
Advertisement
Dr. Tang, Director of Clinical Genomics and cardiology staff, emphasized in the symposium that heart involvement in EGPA carries a major prognostication. The presence of cardiomyopathy is associated with worse prognosis and should always be evaluated when diagnosis of EGPA is confirmed. Cardiac involvement usually warrants more aggressive immunosuppressive therapy, and may occur even when patients do not present with symptoms.
The EGPA Consensus Task Force recommends evaluation for possible heart involvement even when patients are asymptomatic. We routinely assess for cardiac involvement once a diagnosis of EGPA is established. Advances in cardiac imaging have improved the sensitivity of detecting earlier cardiac involvement.
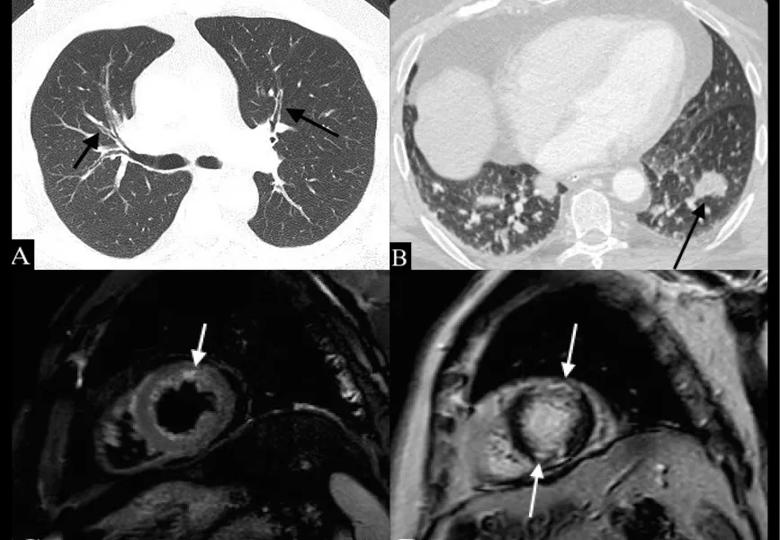
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/bedd585a-40a7-4c91-aa12-902cde55763d/17-RHE-1036-Hajj-Ali_InDesign-File-for-CQD_jpg)
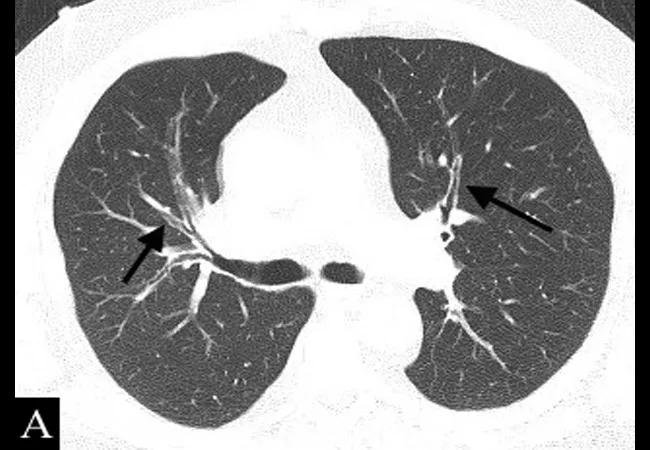
A 54-year-old man with EGPA and lung and cardiac involvement. A: Axial CT image shows diffuse bronchial wall thickening (arrows). B: CT image on the same patient 3 months later shows a new peribronchial nodular opacity in the left lower lobe (arrow); these fleeting opacities are typical of EGPA. C: T2 STIR short-axis Cardiac MR image shows increased signal in the distal anterior wall suggestive of myocardial inflammation (arrow). D: Corresponding phase-sensitive inversion recovery (PSIR) delayed enhancement MR short-axis image shows mid-myocardial enhancement in the apical anterior and inferior segments consistent with myocarditis (arrows). Image and caption republished with permission from Elsevier from Mahmoud S, Ghosh S, Farver C, et al. Pulmonary vasculitis: Spectrum of imaging appearances. Radiol Clin N Am. 2016;54:1097-1118.]
Advertisement
As controlled trials in EGPA are sparse, diagnostic and therapeutic principles are often adapted from other ANCA-associated vasculitides. During the symposium, Michael Wechsler, MD, MMSc, Professor of Medicine at National Jewish Health, shared major advances in the pathogenesis in EGPA. Dr. Wechsler discussed the role of Interleukin 5 (IL5) in EGPA. Higher IL5 levels have been found in EGPA-cultured eosinophils as compared with controls; IL5 is also important in promoting eosinophil adhesions to vascular endothelium.
These findings led to a multisite clinical trial in which Cleveland Clinic participated. This randomized, double-blind, phase 3 study investigated the efficacy and safety of mepolizumab, an IL5 inhibitor, in treating relapsing or refractory EGPA (MIRRA). The MIRRA study is the first placebo-controlled study testing the use of mepolizumab as a steroid-sparing agent in EGPA.
Data from the MIRRA trial is being analyzed, and if the results are positive, it will be a breakthrough in the treatment of EGPA. As difficult as this disease can be to classify and diagnose, it has also proved difficult to treat. We are cautiously hopeful for a breakthrough for our patients.
Dr. Hajj-Ali is Associate Director of the Center for Vasculitis Care and Research. Dr. Tang is Director of the Center for Clinical Genomics.
Advertisement
Advertisement

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Multimodal evaluations reveal more anatomic details to inform treatment

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more