IV thrombolysis should not be delayed because of planned thrombectomy
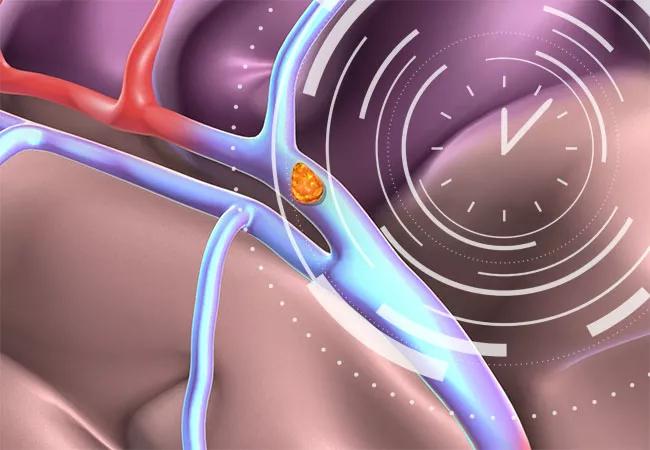
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/1ed6fbce-c294-4453-8616-a4945c55d63f/23-NEU-3936062-CQD-Hero-650x450-1_jpg)
23-NEU-3936062-CQD-Hero-650×450
Faster door-to-needle (DTN) times for intravenous thrombolytic therapy (IVT) are important not only for patients with acute ischemic stroke who are treated with IVT alone but also for those who may undergo endovascular thrombectomy (EVT). So concludes a large cohort study that provides the first evidence that earlier IVT administration for those who ultimately have EVT is associated with better long-term functional outcomes and lower mortality at one year. The study was published in Circulation.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“All eligible candidates for IVT should receive it as soon as possible after onset of stroke symptoms,” says lead and corresponding author Shumei Man, MD, PhD, Medical Director of the Thrombectomy-Capable Stroke Center at Cleveland Clinic Fairview Hospital. “Our study found that each 15-minute delay in administering IVT was associated with fewer days a patient can spend at home and more deaths at one year, regardless of whether patients underwent EVT.”
Although DTN time for IVT has been established as a critical variable in stroke outcomes and thus is an important target of quality initiatives, whether it is also relevant for patients destined to have EVT has been uncertain.
Six randomized clinical trials have tried to demonstrate that EVT alone is not inferior to combined IVT+EVT treatment, but the results were inconclusive. Some experts argue that IVT delays EVT and increases the risk of bleeding and therefore should be skipped or delayed in order to expedite access to an EVT-providing hospital. Dr. Man notes, however, that this argument is based on the inconclusive trial results and the understanding that modern EVT technology is very effective in opening large-artery occlusions. It does not account for the time-dependent benefit of IVT or the possibility that IVT and EVT may have synergistic effects. The trials were not powered sufficiently to account for the time-dependent effect of IVT, she adds, and the trials’ workflows may have delayed thrombolytic administration due to patient consent and randomization. “Furthermore, research has suggested that systemic thrombolysis facilitates early recanalization of the thrombectomy procedure and that the recanalization of large vessels by EVT facilitates IVT to lyse distal or hard-to-reach clots,” Dr. Man says.
Advertisement
Without quality data, clinical decisions based on assumptions may lead to missed treatment opportunities and greater mortality and long-term disability. “The time-dependent benefit of both IVT and EVT and their potential complex interaction make it difficult for clinical trials to fully answer this question,” Dr. Man observes. “It has been proposed that a well-designed patient-level data analysis is needed to address this important issue.”
To meet these challenges and needs, Dr. Man and several thought leaders conceptualized the current large cohort study by linking the U.S. Medicare database with the American Heart Association/American Stroke Association’s Get With The Guidelines Stroke (GWTG-Stroke) registry, which collects important clinical information relevant to care quality, treatment timeliness and patient outcomes. This enabled assessment of the impact of DTN times on outcomes of patients who received IVT only or combined IVT+EVT treatment. Outcomes of patients who underwent only EVT treatment were also compared with outcomes in those who received combined treatment.
The overall cohort consisted of Medicare enrollees treated for acute ischemic stroke from hospitals participating in the GWTG-Stroke quality improvement program. Patients were selected if they received IVT within 4.5 hours or EVT within 7 hours after symptom onset during the period 2015-2018. The final analysis consisted of:
Advertisement
The prespecified primary outcome was home time at 90 days and at one year after stroke. Home time was defined as the number of days alive and not in a healthcare facility. A novel and validated functional outcome measure, home time has been identified from patient surveys as most meaningful to stroke survivors.
For patients treated with both IVT and EVT (after adjusting for patient and hospital factors, including onset-to-EVT times) each 15-minute increase in DTN time for IVT was significantly associated with the following outcomes at one year:
For patients treated only with IVT, shorter DTN times for IVT were also associated with significantly more days at home and significantly lower mortality and readmission at one year.
As DTN times shortened (to ≤ 60, 45 and 30 minutes), patients treated with combined IVT and EVT had incrementally better functional outcomes compared with patients treated with EVT alone. Patients receiving IVT within these time windows had significantly more home time in a year and greater functional independence at discharge and 90 days. These benefits dissipated with DTN times longer than 60 minutes.
“This study shows that delay in IVT is associated with worse functional outcomes and higher mortality even after EVT,” Dr. Man observes. She emphasizes that the study provides important new information on the impact of DTN times for IVT among patients who also undergo EVT, overcoming some of the challenges of randomized clinical trials to address this issue. She notes that the results were based on real-world data with a patient population an order of magnitude larger than typically used in clinical trials for reperfusion therapies.
Advertisement
“These results confirm the view that although EVT is highly effective for recanalization, and that IVT alone usually fails to recanalize an occluded artery, IVT remains an important therapy for EVT candidates,” says Dr. Man. “Even in this EVT era, prompt IVT should remain a critical quality improvement focus of hospital programs, as should moving quickly from IVT to EVT when appropriate.”
Advertisement
Advertisement
The relationship between MTHFR variants and thrombosis risk is a complex issue, but current evidence points to no association between the most common variants and an elevated risk
Pinpointing how tumors reprogram platelets and trigger blood clots
Multi-site study reveals surprising findings
OCEANIC-STROKE results represent long-sought advance in secondary stroke prevention
Aim is for use with clinician oversight to make screening safer and more efficient
Tasked-based therapy improves social connection and quality of life
LAA closure may be compelling option in atrial fibrillation ablation patients at high risk of both stroke and bleeding
Case illustrates essentials of the low-risk, high-potential procedure when paired with rehab