1-Minute Consult

By John A. Zambrano, MS, MHS and Bartolome Burguera, MD, PhD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
By using a pre-visit questionnaire that zeroes in on weight history, eating habits, and level of physical activity, effective obesity counseling can fit into a 20-minute appointment. This information will lay the foundation for effective weight loss counseling and interventions consistent with intensive behavioral therapy for obesity, reimbursable by Medicare.1
We offer the following targeted approach to counseling, achievable within the context of a primary care visit and based on recent evidence, including the 2013 joint guidelines for the treatment of obesity of the American College of Cardiology, the American Heart Association Task Force on Practice Guidelines, and the Obesity Society.2
Measure the patient’s height and weight with the patient wearing light clothing and no shoes, and calculate the BMI as the weight in kilograms divided by the square of the height in meters. A BMI of 30 kg/m2 or greater defines obesity.
According to the 2013 joint guidelines,2 when obtaining a thorough obesity history, the physician should do the following:
This information can be obtained in advance of an office visit through either an electronic medical record portal or a pre-visit questionnaire.
Advertisement
Also assess the patient’s risk of cardiovascular and obesity-related comorbidities. The waist circumference for patients with a BMI between 25 and 35 kg/m2 provides additional information on risk: e.g., a waist circumference greater than 88 cm for women and greater than 102 cm for men indicates increased cardiometabolic risk.2
Use a shared decision-making process to arrive at a set of incremental goals centered around the following evidence-based targets2:
Use motivational interviewing techniques along with the obesity history to negotiate goals. Exercise-related goals should consider the patient’s cardiovascular and musculoskeletal comorbidities.
The most effective weight loss treatment consists of in-person consultations in which comprehensive lifestyle interventions are included. The components of an effective intervention (Table 1) include a reduced-calorie diet, aerobic physical activity, and behavioral strategies to meaningfully support these changes.2
We recommend addressing potential barriers to initiating and maintaining weight-loss interventions, and revisiting them during follow-up visits. Barriers include the following:
Adults with depression are more likely to be obese than adults without depression, and the age-adjusted percentage of adults who are obese increases as depression severity increases.11
Advertisement
Limited access to healthy food choices can lead to poor diets and higher levels of obesity.12 Local grocery store websites and nutrition specialists can help identify a range of healthy and affordable food to sustain a dietary intervention.
Certain diabetic medications, contraceptives, tricyclic antidepressants, atypical antipsychotics, antiseizure drugs, and glucocorticoids promote weight gain and may have alternatives that do not promote weight gain.13
The literature supports frequent in-person sessions as the basis for a successful weight loss intervention (ie, ≥ 14 sessions in 6 months).2 Medicare beneficiaries are eligible for 14 covered visits in the first 6 months and become eligible for an additional monthly visit over the course of 6 subsequent months if a weight loss goal of 3 kg is met in the first 6-month period.
Nutritionists, dieticians, and behavioral psychologists are often instrumental in comprehensive weight loss interventions. Antiobesity drugs help curb appetite, promote weight loss, help enhance adherence to lifestyle modifications, and make it easier for patients to start a program of physical activity.14
The joint 2013 guidelines2 recommend referral for bariatric surgery for adults with a BMI 40 kg/m2 or higher, or for adults with a BMI 35 kg/m2 or higher and obesity-related comorbidities who have not responded to behavioral treatment (with or without pharmacotherapy).
A growing body of evidence promotes the use of group support sessions such as shared medical appointments to encourage healthy eating and physical activity.15
Advertisement
To receive reimbursement from Medicare for obesity counseling, the information listed under “assess” and “advise” in Table 1 should be obtained in the initial visit; and follow-up visits should be used to address items under “agree,” “assist,” and “arrange.” Up to 20 visits are eligible for reimbursement when patients meet the goal of a 3-kg weight loss in the first 6 months (or 14 visits).
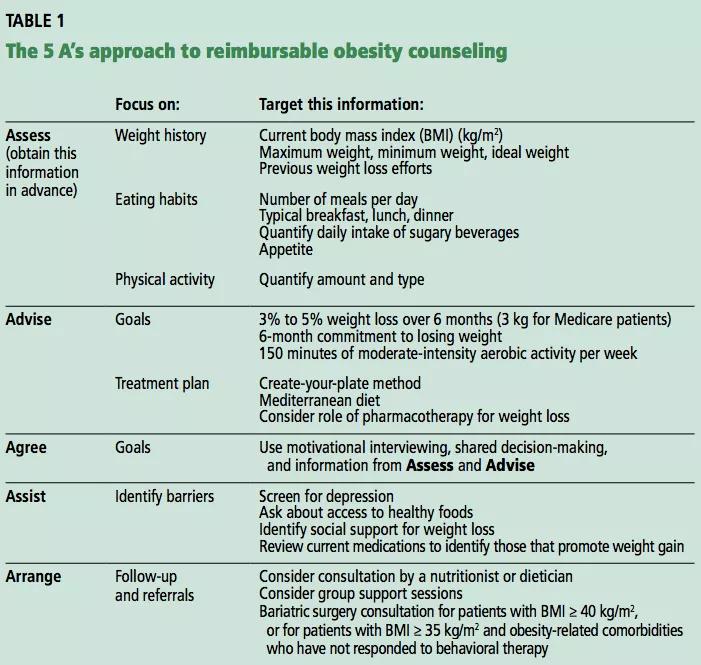
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/328ed1db-25a9-4405-9652-50386a661f65/5-As_Obesity_CCJM_png)
Table 1 displays a targeted counseling approach integrating the 5-A framework (assess, advise, agree, assist, arrange), as described in the Medicare requirements for reimbursable intensive behavioral therapy.1,2Based on our experience, this approach can be easily achieved in the 20-minute appointment when the relevant information is collected in advance of the visit.
More than one-third of US adults are obese.3 And even though the rate of obesity in adults has leveled off since 2009,3 more needs to be done to bend the arc of the national obesity trend. Clinicians tend to focus on the complications of obesity (coronary artery disease, type 2 diabetes, hypertension, hyperlipidemia) rather than on early identification and intervention of obesity itself.4–6 A national study of outpatient visits showed that only 29% of visits by patients who were obese according to their body mass index (BMI) had a documented diagnosis of obesity, suggesting a profound underdiagnosis of obesity.7 According to one study, primary care doctors lack the level of comfort and counseling experience needed to provide obesity and weight loss counseling.8 Yet recent changes to Medicare reimbursement encourage obesity screening and management by covering up to 20 visits for intensive behavioral therapy to treat obesity.1
Advertisement
This article originally appeared in Cleveland Clinic Journal of Medicine. 2017 November;84(11):835-837
References
Advertisement

Pheochromocytoma case underscores the value in considering atypical presentations

Advocacy group underscores need for multidisciplinary expertise

A reconcilable divorce

A review of the latest evidence about purported side effects

High-volume surgery center can make a difference

Advancements in equipment and technology drive the use of HCL therapy for pregnant women with T1D

Patients spent less time in the hospital and no tumors were missed

A new study shows that an AI-enabled bundled system of sensors and coaching reduced A1C with fewer medications