Case series demonstrates successful retreatment of this rare emergency
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/734a212f-52c9-4b3c-912f-f9382021269c/22-NEU-3366031-CQD-Hero-650x450-1_jpg)
22-NEU-3366031-CQD-Hero-650×450
Complete occlusion of intracranial mycotic aneurysms that ruptured despite prior treatment with endovascular coiling was achieved in three patients at Cleveland Clinic using flow-diverting stents, with no associated periprocedural complications or neurological deficits. Details of the cases and their treatment were recently published in Operative Neurosurgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Data regarding the off-label use of flow diverters for intracranial mycotic aneurysms are extremely scarce, given the rarity of this condition,” says Ahmed Kashkoush, MD, a neurosurgery resident at Cleveland Clinic and first author of the report. “This series indicates that flow diversion is a viable salvage option for such aneurysms that are refractory to previous endovascular coiling.”
So-called mycotic or infectious intracranial aneurysms are believed to usually develop from bacterial seeding of a preexisting arterial injury. They are very rare, accounting for no more than 5% of intracranial aneurysms. These highly unstable aneurysms are usually treated with liquid embolization for aneurysm and parent vessel sacrifice, although endovascular coiling, open surgical clipping or parent vessel occlusion with or without bypass can be considered.
Flow-diverting stents are conventionally used for unruptured aneurysms of the internal carotid artery proximal to the posterior communicating artery. But they are increasingly reported to be used off-label for aneurysms located in the posterior circulation as well as for acutely ruptured aneurysms. Until now, published data on the treatment of intracranial mycotic aneurysms with flow-diverting stents were limited to three case reports, all involving unruptured aneurysms.
The current case series was drawn from a database of cerebrovascular procedures performed at Cleveland Clinic between 2017 and 2021. Three cases (with patients aged 45, 33 and 24 years) were identified that involved use of a flow diverter for treatment of a total of four intracranial mycotic aneurysms. The aneurysms were in locations where usual treatment with liquid embolic agents was not feasible due to their proximal location in the vascular tree and risk of large stroke from parent vessel sacrifice. Two aneurysms were located along the middle cerebral artery bifurcation: one was at the posterior cerebral artery P1/2 junction, and the other was at the basilar artery apex. All had ruptured at some point after initial treatment with coil embolization.
Advertisement
A Pipeline™ embolization device was used for the flow-diverting stent in all cases, placed with a transradial or transfemoral approach. After deployment, diagnostic cerebral digital subtraction angiography was used to assess adequate stasis and to check for kinking, endoleak or parent vessel occlusion.
All aneurysms demonstrated complete occlusion at long-term angiographic follow-up, and no patients developed new complications or neurological deficits. Representative imaging studies from one of the patients are presented in the figure.
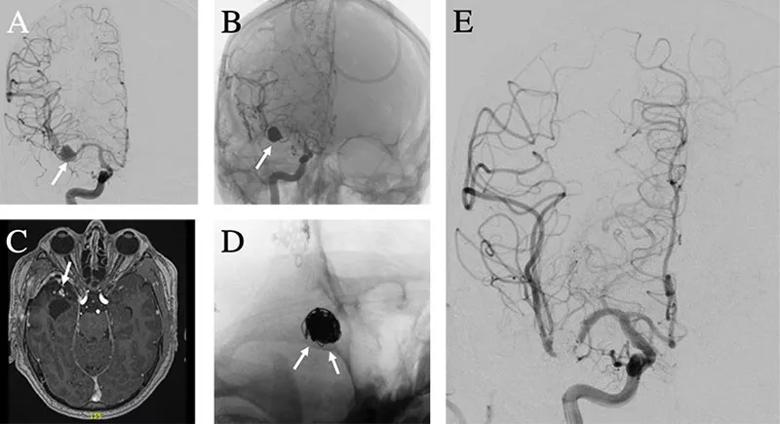
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c5a24587-2d14-4e90-a9d7-664075795580/22-NEU-3366031-CQD-Inset-800x435-1_jpg)
Figure. Case illustration of flow-diverting stent use in mycotic aneurysm. (A) A right middle cerebral artery mycotic aneurysm (arrow) was found on a workup of intracerebral hemorrhage in a patient with infective endocarditis. (B) The aneurysm was successfully treated with balloon-assisted coil embolization (arrow) without residual flow into the aneurysm. (C) Magnetic resonance angiography three months later demonstrated residual contrast enhancement at the neck and in the aneurysm lumen suggestive of coil compaction and aneurysmal recurrence (arrow). (D) A flow-diverting stent was successfully placed across the aneurysm neck (arrows). (E) Follow-up angiography at 11 months demonstrated no residual flow into the aneurysm.
“Intracranial mycotic aneurysms are rare, with no evidence-based guidelines for their management,” says Cleveland Clinic vascular neurosurgeon Mark Bain, MD, the paper’s senior author. “Treatment must be handled on a case-by-case basis, considering rupture status, aneurysm size and progression, and mass effect from intraparenchymal hemorrhage.”
Advertisement
The group’s case series report outlines the general management strategies neurosurgeons use at Cleveland Clinic, which are summarized below.
For uncomplicated small, unruptured mycotic aneurysms, antibiotics can be tried as initial therapy. More advanced treatment is indicated for those that are ruptured or progressing despite antibiotics, or if the patient must be on anticoagulation therapy for another condition.
For flow diversion, the patient is placed on dual antiplatelet therapy, which is continued for three months for anterior circulation aneurysms and six months for aneurysms of the posterior circulation. After this period, aspirin monotherapy is continued indefinitely. Antibiotic therapy (six to eight weeks) is prescribed to mitigate risk of stent infection.
Open surgical approaches can also be used, although surgical reconstruction is particularly difficult for these very delicate lesions and thin blood vessels that are especially prone to rupture and tearing intraoperatively.
“Proximal mycotic aneurysms, such as the ones in this series, are especially challenging, with fewer treatment options,” Dr. Bain observes. “In such cases, we have to be creative in considering novel approaches.”
All cases in this study involved initial treatment of a proximal mycotic aneurysm with coiling, calling into question the wisdom of this initial strategy. Although it appears that coiling leaves the aneurysm vulnerable to future rupture, the authors note that it may still be a reasonable choice acutely after rupture to minimize immediate risk.
Advertisement
“Monitoring with angiography post-coiling is needed to check for growth or rupture,” says Dr. Bain. “For recurrence, placement of a flow-diverting stent should be considered, ideally after any other needed invasive operations are over and the patient can safely begin antiplatelet therapy.”
Because of the multiple treatments used for this condition and the heterogeneity of lesion location, multiple questions remain about optimal therapy.
“This condition is rarely seen, so it’s unlikely we will see rigorous randomized controlled trials to guide management,” concludes Dr. Kashkoush. “However, prospective and multicenter studies would be useful to establish long-term safety and efficacy of different treatment approaches.”
Advertisement
Advertisement
Evolving thinking on when and how to treat brain aneurysms and AVMs
Quick and aggressive responses to multiple complications have led to remarkable recovery
Cleveland Clinic findings prompt efforts for broad data pooling
Guidance from the largest cohort of SEEG-confirmed insular epilepsy patients reported to date
Ethical guidance provides guardrails so medical advances benefit patients
OCEANIC-STROKE results represent long-sought advance in secondary stroke prevention
Two studies from Cleveland Clinic may help advance the technology toward broader clinical use
Distinct MRI signature includes lesions beyond the corpus callosum, features predictive of vision and hearing loss