Cleveland Clinic findings prompt efforts for broad data pooling

Researchers at Cleveland Clinic have identified an apparent increased risk for intracranial aneurysm (IA) among people with Marfan syndrome in the largest review of IA in this population reported to date. The retrospective study was published in the Journal of Vascular Surgery (2023;76[3]:633-637).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
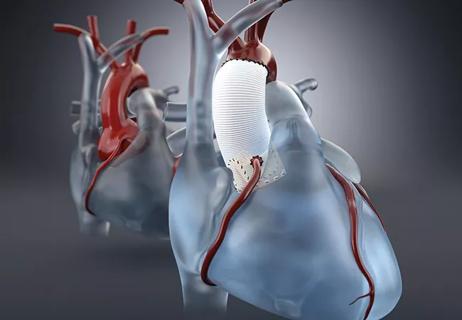
The relationship between Marfan syndrome and aneurysmal pathology of the aorta is well established. But despite both epidemiologic and genetic evidence linking aortic and intracranial aneurysms, virtually no data existed previously on the risk for IA among people with Marfan syndrome, an autosomal dominant connective tissue disorder affecting 2 to 3 per 10,000 population.
“It’s difficult to do a large-scale study because Marfan syndrome is so uncommon,” says Cleveland Clinic vascular surgeon David Laczynski, MD, first author of the study. “We’re fortunate here at Cleveland Clinic to have such a wide net to be able to study these patients.”
Of 983 total patients with Marfan syndrome seen at Cleveland Clinic between 1995 and 2021, 198 had undergone intracranial imaging and constituted the study cohort. Review of those cases revealed that 14 patients (7.1%) had an IA. In contrast, the prevalence of IA in the general population is approximately 1%.
Because IAs are usually fatal or cause lifelong disability, the findings strongly suggest consideration of routine intracranial imaging in people with Marfan syndrome, the researchers conclude. But they note that more data are needed before an official recommendation can be made.
“These patients are already undergoing multiple imaging studies, so getting an additional image of the head doesn’t seem unreasonable,” Dr. Laczynski says. “We look extensively at their risk of aneurysm in every other vascular bed, but not in the head. If anything, this is a call for other centers to pull their data together and take a look.”
Advertisement
The 131 male and 67 female patients in the study cohort had a mean age of 52.7 years. They underwent either intracranial CT angiography (69.2%) or magnetic resonance angiography (31.3%).
Most of these scans were done for routine preoperative imaging prior to aortic or cardiac repair, or out of suspicion of a cerebrovascular accident. There was no evidence that any had been performed solely for suspected IA, thereby reducing ― although not eliminating ― the likelihood of selection bias, Dr. Laczynski points out.
Among the study cohort, 29% had type A aortic dissections, 14% type B dissections and 38% abdominal aortic aneurysms. Most (81%) had undergone a prior thoracic aortic surgical repair.
Of the 14 patients found to have an IA, four had more than one. The largest share of IAs (43%) were in the internal carotid artery, while another 29% each were in the vertebral and basilar arteries.
Mean IA size was 7.0 mm, with the maximum size 22.0 mm. One patient (the one with the 22.0-mm aneurysm) underwent surgical IA repair. For the general population with an IA, the neurosurgery literature suggests that repair is indicated for aneurysms 8 mm or larger, Dr. Laczynski notes.
None of the patients experienced aneurysm rupture during mean follow-up of 5.3 years.
Further analysis showed no specific patient characteristics that might predict an IA. Those with and without IAs did not differ by age, presence of obesity, ascending or descending aorta diameter, or rates of abdominal aortic aneurysm.
Advertisement
The next step, Dr. Laczynski says, is to enlist other institutions to gather and pool their data in order to determine support for an official recommendation for intracranial imaging in the setting of Marfan syndrome. For this, he and his Cleveland Clinic colleagues will turn to the Vascular Low Frequency Disease Consortium (VLFDC), which comprises more than 75 institutions and 135 investigators from the U.S. and abroad.
The team aims to submit a proposal by the end of the year to the VLFDC for pooling data on IAs in patients with Marfan syndrome, with Cleveland Clinic’s Cardiovascular Marfan & Connective Tissue Clinic serving as lead center.
If the pooled data reinforce the increased risk found in the Cleveland Clinic population, the hope is that multiple professional societies would jointly issue a recommendation for routine intracranial imaging. “The first step might be expert consensus from leaders in the field stating that the benefits outweigh the risks, if we don’t have level 1 evidence to support a guideline,” Dr. Laczynski explains.
“Marfan patients may need to be considered for screening for intracranial aneurysms just as we routinely screen patients with Loeys-Dietz syndrome,” says cardiologist and study co-author Vidyasagar Kalahasti, MD, Director of the Cardiovascular Marfan Syndrome & Vascular Connective Tissue Disorders Clinic in Cleveland Clinic’s Aorta Center. “However, this study only incorporated patients who had CTA or MRA of the brain prior to an elective thoracic aortic repair, and this may have led to somewhat higher prevalence of intracranial aneurysms relative to the general population. It is important to review data from other institutions to get a true understanding of the prevalence. This will enable recommendation change and help with updating guidelines.”
Advertisement
Study co-author Francis Caputo, MD, concurs. “The correlation between intracranial aneurysm and those Marfan patients afflicted with aortic aneurysms is poorly understood,” says Dr. Caputo, Vascular Surgery Director of Cleveland Clinic’s Aorta Center. “To better understand the prevalence and risk, a multi-institutional study is needed to fully elucidate the correlation.”
Improvements in cardiac care over recent decades have dramatically lengthened the typical life expectancy of people with Marfan syndrome, from the mid-40s into the 70s today, a level not much lower than that of the general population.
“Despite these advances,” Dr. Laczynski notes, “Marfan’s is a lifelong disease that these patients suffer with, and they need a comprehensive multispecialty team monitoring and working with them. We hope to continue to push the boundaries of what we know about this disease and continue to give these patients the best care possible.”
Advertisement
Advertisement

When to recommend aortic root surgery in Marfan and other syndromes

Evolving thinking on when and how to treat brain aneurysms and AVMs

Quick and aggressive responses to multiple complications have led to remarkable recovery
Many young patients can avoid lifelong anticoagulation with a valve-sparing approach

Case series demonstrates successful retreatment of this rare emergency

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR