GIAI is common in patients treated with glucocorticoids
This has been adapted from an article originally published in Cleveland Clinic Journal of Medicine, Vol. 91, April 2024. The original can be found here.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
By Noura Nachawi, MD, Dingfeng Li, MD, and M. Cecilia Lansang, MD, MPH
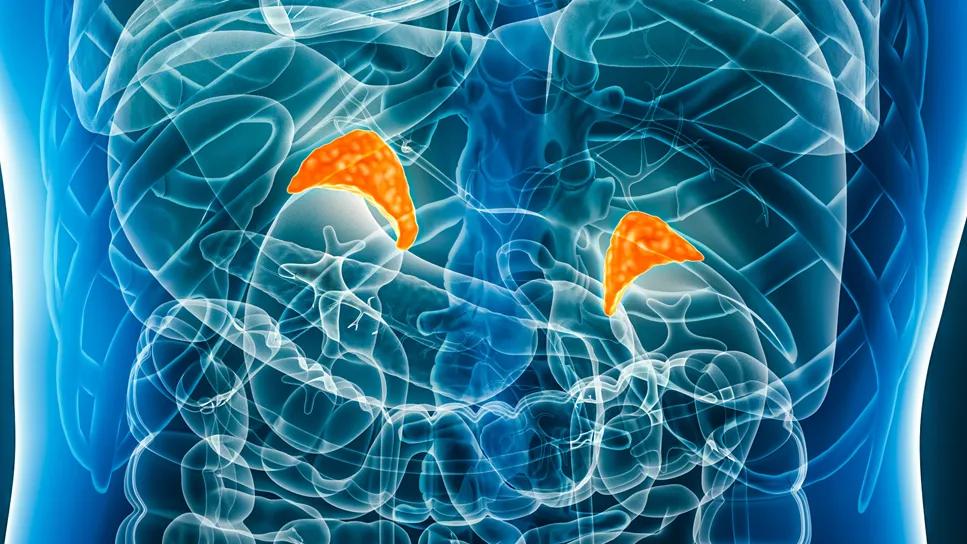
Glucocorticoid-induced adrenal insufficiency (GIAI) is a well-known side effect of glucocorticoid therapy, and clinicians usually expect it in patients who receive systemic (oral, intravenous and intramuscular) glucocorticoids in doses equivalent to more than 5 mg of prednisone for at least three weeks.
However, glucocorticoids given through other routes can also suppress the adrenal glands. Unfamiliarity with GIAI, especially when caused by non-systemic formulations of glucocorticoids, can lead to delay in diagnosis or misdiagnosis and lack of proper patient education. This lack of awareness often leads to failure to implement an adrenal action plan and underuse of injectable glucocorticoids at home or, in cases of adrenal crisis, in the emergency room.
Ultimately, gaps in care in managing adrenal suppression often worsen clinical outcomes and quality of life in this vulnerable patient population, who tend to have a poor quality of life at baseline. This review highlights the differences between primary adrenal insufficiency, secondary adrenal insufficiency (including GIAI) and glucocorticoid withdrawal syndrome.
The adrenal cortex produces three main types of hormones:
Advertisement
Primary adrenal insufficiency
Diseases of the adrenal cortex can lead to primary adrenal insufficiency, with insufficient production of glucocorticoids, mineralocorticoids or both. The prevalence of primary adrenal insufficiency in the United States is not well documented. However, it is rising in Europe, where it has been reported to be as high as 22.1 per 100,000 population.
Autoimmune adrenalitis (also known as Addison disease, for Thomas Addison, who first described it in 1855) is the most common cause of primary adrenal insufficiency in developed countries. Other causes include tuberculosis, human immunodeficiency virus infection, trauma, and use of immune checkpoint inhibitors.
Secondary adrenal insufficiency
Secondary adrenal insufficiency occurs when the hypothalamus does not produce enough corticotropin-releasing hormone or the anterior pituitary gland does not produce enough adrenocorticotropic hormone so that the adrenal cortex is not stimulated and does not produce enough glucocorticoids. Mineralocorticoid secretion, however, is usually preserved, as the renin-angiotensin-aldosterone system, involving the cardiovascular and renal systems, is not affected.
Therefore, patients with secondary adrenal insufficiency are less likely to have hypotension than those with primary adrenal insufficiency.
Adrenal insufficiency caused by suppressed corticotropin-releasing hormone is sometimes called tertiary adrenal insufficiency. However, this term remains controversial. Here, we will use secondary adrenal insufficiency for both pituitary and hypothalamic causes of adrenal insufficiency.
Advertisement
Secondary adrenal insufficiency is more common than primary, with an estimated prevalence of up to 28 per 100,000 people. Common causes include pituitary tumors, other tumors metastasizing to the pituitary gland, and head trauma.
Other important causes are the many drugs that can affect the hypothalamic-pituitary-adrenal axis (HPAA) at different levels. The drugs that primary care clinicians most often encounter are immune checkpoint inhibitors, opioids and glucocorticoids. Secondary adrenal insufficiency caused by emerging immunotherapies such as monoclonal antibody targeting programmed cell death protein 1 (PD-1; nivolumab and pembrolizumab) and monoclonal antibody targeting cytotoxic T-lymphocyte antigen 4 (CTLA-4; ipilimumab) are also common, more so when these agents are used in combination or sequence. Of note, these medicines can also cause primary adrenal insufficiency, though infrequently.
Opioids are believed to suppress the adrenal glands by binding to receptors in the hypothalamus and pituitary, exerting tonic inhibition on the HPAA. Opioid-induced adrenal insufficiency is estimated to affect approximately 15% of patients treated with opioids for at least three to six months. Li et al1 reported that 9 (9%) of 102 patients who were receiving more than 20 morphine milligram equivalents per day developed adrenal insufficiency. All were treated with glucocorticoid replacement while weaning off opioids until their HPAA recovered, which occurred within one to 14 months of stopping the opioid. Glucocorticoid replacement improved pain, quality of life and physical function.
Advertisement
Glucocorticoids are powerful anti-inflammatory agents used to treat autoimmune and other conditions. However, long-term use in supraphysiologic doses can suppress the HPAA and consequently cause GIAI.
GIAIis a fairly new term and has been used by some authors interchangeably with adrenal suppression. Other authors use the term more specifically to describe symptoms in patients with HPAA suppression who receive inadequate treatment with glucocorticoids during stressful situations. The rest of the discussion will focus on GIAI, given that exogenous glucocorticoid use is the most common cause of adrenal suppression.
In a systematic review and meta-analysis of 73 studies, the median prevalence of GIAI was 37% in patients receiving any form of glucocorticoids. In another meta-analysis, the median prevalence was 48.7% in those receiving oral glucocorticoids and 52.2% in those receiving intra-articular injections.
Excessive glucocorticoids, whether endogenous due to adrenal lesions secreting excessive cortisol or from an exogenous source, bind to receptors in the hypothalamus and pituitary, triggering negative feedback on adrenocorticotropic hormone release. Chronic suppression of adrenocorticotropic hormone eventually leads to atrophy of the zona fasciculata but not the zona glomerulosa, resulting in impaired cortisol secretion but intact mineralocorticoid secretion.
Risk factors for GIAI
Although high-quality evidence is lacking, available data suggest that many factors affect the risk of GIAI, including glucocorticoid dose, duration, formulation, frequency and timing of administration, pharmacokinetics interaction with other medications, and cushingoid features.
Advertisement
Glucocorticoid dose and duration. In studies in patients with asthma, GIAI occurred in 2.4% of those treated with low doses of systemic glucocorticoids, 8.5% of those receiving medium doses, and 21.5% of those receiving high doses. Short-term use (< 1 month) resulted in GIAI in 1.4%, medium-term use (one month to one year) resulted in GIAI in 11.9%, and long-term use (> 1 year) resulted in GIAI in 27.4%. The patterns were similar in patients treated only with inhaled glucocorticoids. However, other studies have found no correlations between glucocorticoid dose or duration and risk of GIAI.
Formulation. Dexamethasone is 25 times more potent than hydrocortisone, and prednisone is four times more potent. Duration of effect is more than 36 hours for dexamethasone, 18 to 36 hours for prednisone, and 8 to 12 hours for hydrocortisone. At equivalent doses (0.75 mg of dexamethasone is equivalent to 5 mg of prednisone or 20 mg of hydrocortisone), dexamethasone has stronger suppressive effects on the HPAA compared with hydrocortisone. However, studies have not shown any difference in HPAA suppression in patients treated with equivalent doses of prednisone compared with dexamethasone.
Frequency and timing of administration. Pulse therapy with high-dose glucocorticoids (eg., intravenous methylprednisolone 250–500 mg weekly for 6–12 weeks) and alternate single-day dosing are less likely to cause GIAI compared with bedtime dosing and frequent dosing (more than once daily). GIAI after short bursts of glucocorticoids (7–14 days) has been infrequently reported, particularly in patients with chronic obstructive pulmonary disease who receive frequent short bursts of glucocorticoids and patients with malignancies who receive bursts of dexamethasone to mitigate chemotherapy-related nausea.
Interactions with other medications. Concomitant use of glucocorticoids and hepatic cytochrome P450 3A4 inhibitors (eg., protease inhibitors, azoles, clarithromycin, erythromycin) increases the levels of active metabolites of glucocorticoids, and, consequently, the risk of GIAI. This happens with all glucocorticoid formulations metabolized by cytochrome P450 3A4 regardless of route of administration: oral, injectable, intra-articular, and even inhaled and intranasal formulations. Primary care clinicians should be aware of these interactions when they suspect GIAI, especially in patients with chronic obstructive pulmonary disease or human immunodeficiency virus infection.
Cushingoid features. A cushingoid appearance usually indicates that the glucocorticoid dose is excessive. Some authors have indicated that patients with cushingoid features while on glucocorticoids are at a very high risk for GIAI.
Unrecognized sources of exogenous glucocorticoids. Inhaled glucocorticoids bind to receptors in the lungs, mouth and oropharynx, leading to systemic exposure and possibly HPAA suppression.
Intra-articular and epidural injections. Systemic absorption of intra-articular glucocorticoids has been widely described. Similarly, HPAA suppression after epidural corticosteroid injections has been reported with multiple formulations, doses and frequencies (after both single and recurrent doses).
Some patients do not know that these injections contain steroids and therefore may not report this exposure if they present with GIAI symptoms. Serum and urine testing for synthetic steroids are important tools when GIAI is suspected. Urine screening for synthetic glucocorticoids (liquid chromatography-tandem mass spectrometry with stable isotope dilution analysis) is reported to detect prednisone and prednisolone for up to 40 days after epidural injections and for up to 62 days after triamcinolone epidural injections.
Topical formulations. Several studies reported GIAI induced by topical cutaneous glucocorticoids.
Eye drops. GIAI due to ophthalmic glucocorticoids has been reported in adult, pediatric and animal studies.
Locally active enteral formulations. Rectal glucocorticoids and oral budesonide are used to treat inflammatory bowel disease. The risk of GIAI is dose- and duration-dependent in patients taking oral budesonide, being higher when patients take more than 6 mg daily for at least eight weeks. GIAI has been reported in patients using prednisolone enemas, whereas beclomethasone dipropionate enemas seem to be safer.
Other medications with glucocorticoid activity. Megestrol acetateis a synthetic progestin with glucocorticoid-like activity commonly used as an appetite stimulant in patients with malignancy and anorexia. Several reports have highlighted the incidence of adrenal insufficiency, Cushing syndrome or both in patients treated with megestrol acetate, specifically, when megestrol acetate is combined with dexamethasone.
Medroxyprogesterone acetate, another progestin that binds glucocorticoid receptors, is used to treat endometrial cancer, endometriosis and abnormal uterine bleeding, and as a contraceptive, and is reported to cause HPAA suppression.
Excessive endogenous hormone secretion or exogenous administration often leads to tolerance (decreased response to the elevated hormones and the need for even higher levels to achieve the same effect) followed by physiologic and psychologic dependence. In this situation, gradually tapering or abruptly stopping the glucocorticoids can induce glucocorticoid withdrawal syndrome, even while patients are still receiving supraphysiologic doses of glucocorticoids. Glucocorticoid withdrawal syndrome manifests as a spectrum of nonspecific symptoms and is mediated by multiple mechanisms.
Chronic suppression of corticotropin-releasing hormone after stopping or tapering from glucocorticoids leads to adrenal insufficiency, adrenal crisis, depressive mood changes, hypersomnia and lethargy. Prolonged suppression of proopiomelanocortin-related peptides causes myalgia, arthralgia, fever and headache. Depressed central noradrenergic and dopaminergic systems cause nonspecific withdrawal symptoms along with anorexia, nausea, vomiting and weight loss. Loss of glucocorticoid’s suppressive effect on calcium absorption results in hypercalcemia and hyperphosphatemia.
These symptoms can develop at any time—during glucocorticoid taper (while the patient is still on supraphysiologic doses), after completely stopping glucocorticoids, and even after there is biochemical evidence of HPAA recovery. Long-term treatment with supraphysiologic doses of glucocorticoids often leads to HPAA suppression and adrenal insufficiency. At the same time, tolerance to and dependence on high doses of glucocorticoids causes glucocorticoid withdrawal syndrome when attempting to taper or discontinue these drugs.
Therefore, adrenal insufficiency and glucocorticoid withdrawal syndrome share similar clinical features; however, they are completely different clinical entities that often overlap until the HPAA recovers. Results of biochemical testing, including early morning cortisol levels and the corticotropin stimulation test, can be normal or suboptimal, and hence, not helpful in making this diagnosis.
Glucocorticoid withdrawal syndrome after successful treatment of Cushing syndrome. Evidence on glucocorticoid withdrawal syndrome in patients with GIAI caused by exogenous glucocorticoid use is lacking. However, several studies have looked into glucocorticoid withdrawal syndrome in patients with GIAI caused by adrenal lesions secreting excessive endogenous cortisol (adrenocorticotropic hormone independent Cushing syndrome). Up to 99% of patients with Cushing syndrome have HPAA suppression.
Patients with Cushing syndrome can develop tolerance to and dependence on excessive endogenous cortisol, and hence, suffer from glucocorticoid withdrawal syndrome postoperatively.76 After resection, glucocorticoid taper is indicated until the HPAA recovers. Postoperative glucocorticoid withdrawal syndrome is usually characterized by biochemical evidence of HPAA suppression, with many signs and symptoms consistent with cortisol deficiency despite the use of supraphysiologic doses of glucocorticoids. Common symptoms include myalgias, arthralgias, fatigue, weakness, sleep disturbance, and mood changes. In a recent prospective observational study, myalgias, arthralgias, and weakness got progressively worse 5 to 12 weeks after surgery. Glucocorticoid withdrawal syndrome can be difficult to differentiate from adrenal insufficiency, which complicates glucocorticoid dosing, and tapering regimens.
In a retrospective study of the postoperative course of 81 patients with adrenocorticotropic hormone independent Cushing syndrome, glucocorticoid withdrawal syndrome was most common when the 8 am serum cortisol level 24 hours after the last glucocorticoid dose was less than 5 μg/dL, whereas no withdrawal symptoms were reported when it was higher than 10 μg/dL.
Assessing and expediting HPAA recovery in GIAI
Currently, there is no consensus on the best approach to assessing HPAA recovery in patients with GIAI and those who have undergone surgery for Cushing syndrome. However, several factors related to the patient’s characteristics, glucocorticoid course of therapy, and biochemical testing could be used to estimate the recovery of the HPAA and help clinicians with their approach to patients with GIAI.
Studies have looked at recovery of the HPAA after successful surgery for endogenous adrenocorticotropic hormone-independent Cushing syndrome, and we could extrapolate some of their conclusions to GIAI.
Slower HPAA recovery is expected in patients treated with higher doses of glucocorticoids, women, patients with lower body mass index, and patients with cushingoid features. Faster recovery (in weeks to months) is reported in patients treated with high doses of oral glucocorticoids for less than 1 month.19 HPAA recovery could take up to 6 to 12 months in patients treated with glucocorticoids for more than 12 months. Future studies are needed to prove the hypothesis.
An observational study by Pofi et al2 involving 776 patients suggested a cutoff of 3.6 μg/dL (using the Roche Modular System) between baseline cortisol and 30-minute cortisol levels after a 250-μg corticotropin stimulation test to predict recovery of the HPAA. If the change in cortisol level is less than 3.6 μg/dL and the random cortisol level is less than 7.2 μg/dL after one year, patients are less likely to recover HPAA function. Switching from a longer-acting glucocorticoid (eg, dexamethasone, prednisone) to a shorter-acting one (eg, hydrocortisone) has been hypothesized to expedite HPAA recovery, but evidence remains inadequate to recommend one glucocorticoid vs others for HPAA recovery.
Corticosteroid taper in patients with GIAI and after surgery for Cushing syndrome. Clinicians should work in multidisciplinary teams and closely monitor conditions that could possibly worsen or relapse due to lowering glucocorticoid doses. Glucocorticoids should be tapered when appropriate to safely induce HPAA recovery while at the same time avoiding glucocorticoid withdrawal syndrome or adrenal crisis.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d07e5d99-3ac8-469a-b5a2-6dc83baf3f42/https-assets-clevelandclinic-org-transform-29e778b1-ef39-4e55-ae28-773d7e5da50f-glucocorticoid-indused-adrenal-insufficiency-chart)
1. Li T, Cunningham JL, Gilliam WP, Loukianova L, Donegan DM, Bancos I. Prevalence of opioid-induced adrenal insufficiency in patients taking chronic opioids. J Clin Endocrinol Metab 2020;105(10):e3766–e3775.
2. Pofi R, Feliciano C, Sbardella E, et al. The short synacthen (corticotropin) test can be used to predict recovery of hypothalamopituitary-adrenal axis function. J Clin Endocrinol Metab 2018;
103(8):3050–3059.
Advertisement

Timing and type of side effects differ greatly from chemotherapy

Surgeons reassured by low risk of harm

Pheochromocytoma case underscores the value in considering atypical presentations

Advocacy group underscores need for multidisciplinary expertise

A reconcilable divorce

A review of the latest evidence about purported side effects

High-volume surgery center can make a difference

Advancements in equipment and technology drive the use of HCL therapy for pregnant women with T1D