Primary hyperparathyroidism is frequently underdiagnosed
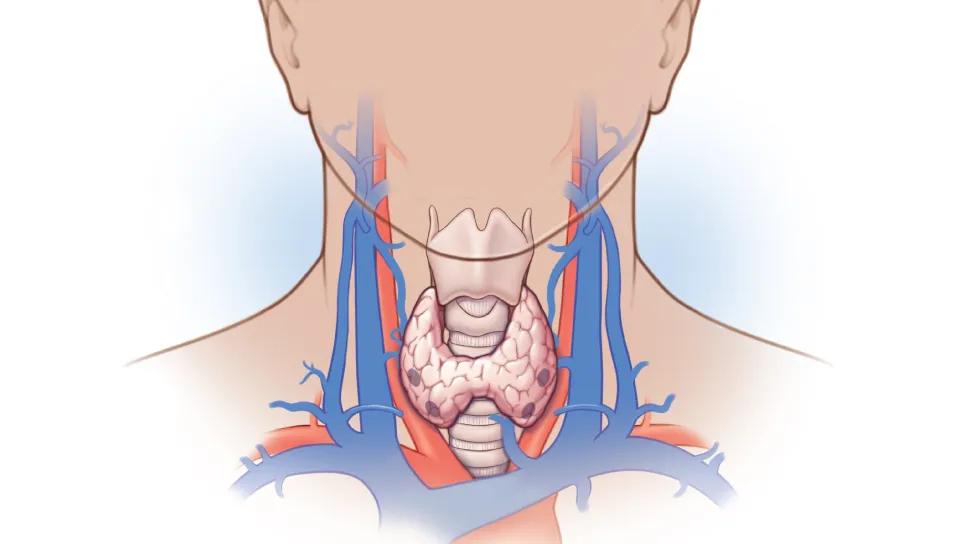
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/7bcbde19-6277-42ce-9de0-f8dbfeebcec8/parathyroidectomy-should-i-refer-patient)
medical illustration of parathyroidectomy
This article was first published in Cleveland Clinic Journal of Medicine and adapted for Consult QD.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
By Gustavo Romero-Velez, MD, Leila Zeinab Khan, MD and Judy Jin, MD
A 60-year-old woman who is otherwise healthy is found to have an elevated serum calcium level of 10.5 mg/dL (reference range 8.5–10.2) during her yearly checkup. Her main complaints are memory loss and fatigue, but she denies prior fractures or kidney stones. Review of her medical record shows that her calcium levels have been persistently elevated for at least the past five years. Additional workup demonstrates a parathyroid hormone level (PTH) of 55 pg/mL (15–65), 25-hydroxyvitamin D level of 40 ng/mL (31–80), and 24-hour urine calcium excretion of 240 mg (100–300). She has known osteopenia, with a T-score of −2.4 at the femoral neck. Her serum creatinine level is normal. Should this patient be referred for parathyroidectomy?
In patients with primary hyperparathyroidism, the decision to refer for surgery should be individualized and not based solely on whether the patient meets guideline criteria. The first question that must be addressed then is whether our patient has primary hyperparathyroidism.
She has hypercalcemia (serum level of 10.5 mg/dL) with a replete 25-vitamin D level, and although her PTH level at greater than 30 pg/mL is within the normal range, it is still inappropriately high, confirming the diagnosis of primary hyperparathyroidism. Traditionally, the diagnosis of primary hyperparathyroidism was made based on concomitant calcium and PTH levels above the normal limits, but we now recognize that what matters is the relationship of the levels rather than the absolute values.1
Advertisement
Also, although the diagnosis is clear in this patient with hypercalcemia and an inappropriately high PTH, familial hypocalciuric hypercalcemia should be considered in the differential. Familial hypocalciuric hypercalcemia, though far less common than primary hyperparathyroidism, presents with similar biochemical patterns, except for hypocalciuria (< 100 mg/24 hours). The urine calcium:creatinine clearance ratio may help distinguish between the two conditions.2

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/9a8ce1ad-18a2-4f9b-a543-e0781088783d/parathyroidectomy-should-i-refer-patient-inset)
The next question—should our patient be referred for parathyroidectomy?—is more complex. Surgery is typically recommended in all patients with at least one of the following:
According to current international consensus guidelines, the patient does not meet the criteria for surgery because her serum calcium is not 1.0 mg/dL above the upper limit of normal, she is older than 50, and she does not have osteoporosis, nephrolithiasis, fractures, decreased creatinine clearance or hypercalciuria.2
Advertisement
The decision to treat, however, should not rely solely on whether the patient meets guideline criteria. Surgery can improve bone health, reduce the likelihood of nephrolithiasis or even chronic kidney disease, and improve serum calcium values. Also, several neuropsychiatric symptoms are likely to improve with surgery, such as fatigue and brain fog.2
Research indicates that the level of hypercalcemia does not correlate with the presence of symptoms.3 Thus, our patient may still be prone to symptoms attributable to primary hyperparathyroidism with her calcium level of 10.5 mg/dL. Her age also may not be relevant and should be seen as being part of a continuum rather than a specific cutoff point. Given current life-expectancy estimates, patients older than age 50 can still be at risk for additional long-term manifestations of the disease. In fact, parathyroidectomy is the most cost-effective strategy for patients with at least three years of life expectancy based on fracture risk reduction.4
Related to bone health, while our patient does not meet the bone mineral density criterion (T-score ≤ −2.5) for surgery, the T-score also should be seen as a continuum. She likely will progress and eventually meet the criterion, as untreated primary hyperparathyroidism can cause significant bone loss.5 Parathyroidectomy can improve bone mineral density and reduce the risk of fractures.5-6
Finally, our patient presented with neurocognitive symptoms that included memory loss and fatigue. Though still a matter of debate, there is growing evidence that these symptoms and quality of life can improve after parathyroidectomy.1,7-8
Advertisement
Careful evaluation of this patient indicates she would benefit from consultation with a high-volume parathyroid surgeon.
Primary hyperparathyroidism is frequently underrecognized and underdiagnosed. It is the most common cause of hypercalcemia in the outpatient setting.9 While consensus guidelines may be useful in large population studies, individualizing care is most important. Surgical correction can result in improvements in health and quality of life. It is essential to recognize hypercalcemia with nonsuppressed PTH values and to individualize treatment for each patient even when the exact surgical criteria are not met. In patients presenting at a young age or with strong family history, hereditary endocrinopathies must be considered.
1. Wilhelm SM, Wang TS, Ruan DT, et al. The American Association of Endocrine Surgeons guidelines for definitive management of primary hyperparathyroidism. JAMA Surg 2016; 151(10):959–968.
2. Bilezikian JP, Khan AA, Silverberg SJ, et al. Evaluation and management of primary hyperparathyroidism: summary statement and guidelines from the fifth international workshop. J Bone Miner Res 2022; 37(11):2293–2314.
3. Boone D, Politz D, Lopez J, Mitchell J, Parrack K, Norman J. Concentration of serum calcium is not correlated with symptoms or severity of primary hyperparathyroidism: an examination of 20,081 consecutive adults. Surgery 2017; 161(1):98–106.
4. Zanocco KA, Wu JX, Yeh MW. Parathyroidectomy for asymptomatic primary hyperparathyroidism: a revised cost-effectiveness analysis incorporating fracture risk reduction. Surgery 2017; 161(1):16–24.
5. Seib CD, Meng T, Suh I, et al. Risk of fracture among older adults with primary hyperparathyroidism receiving parathyroidectomy vs nonoperative management. JAMA Intern Med 2022; 182(1):10–18.
6. Lundstam K, Pretorius M, Bollerslev J, et al. Positive effect of parathyroidectomy compared to observation on BMD in a randomized controlled trial of mild primary hyperparathyroidism. J Bone Miner Res 2023; 38(3):372–380.
7. Pretorius M, Lundstam K, Hellström M, et al. Effects of parathyroidectomy on quality of life: 10 years of data from a prospective randomized controlled trial on primary hyperparathyroidism (the SIPH-Study). J Bone Miner Res 2021; 36(1):3–11.
8. Ambrogini E, Cetani F, Cianferotti L, et al. Surgery or surveillance for mild asymptomatic primary hyperparathyroidism: a prospective, randomized clinical trial. J Clin Endocrinol Metab 2007; 92(8):3114–3121.
9. Press DM, Siperstein AE, Berber E, et al. The prevalence of undiagnosed and unrecognized primary hyperparathyroidism: a population-based analysis from the electronic medical record. Surgery 2013; 154(6):1232–1238.
Advertisement
Advertisement
Pheochromocytoma case underscores the value in considering atypical presentations
Advocacy group underscores need for multidisciplinary expertise
A reconcilable divorce
A review of the latest evidence about purported side effects
High-volume surgery center can make a difference
Advancements in equipment and technology drive the use of HCL therapy for pregnant women with T1D
Patients spent less time in the hospital and no tumors were missed
A new study shows that an AI-enabled bundled system of sensors and coaching reduced A1C with fewer medications